Hiroshi Nakaguchi
Professor, and Director of the Convalescent Rehabilitation Center, International University of Health and Welfare Atami Hospital
Japan Neurosurgical Society Specialist / Preceptor
Japan Neurosurgical Society Academic Councilor
Member of the International Federation of Neurosurgeons (WFNS)
Member of the Asian and Australasia Neurosurgical Society (AASNS)
Japanese Stroke Society Specialist / Preceptor
Japanese Society for Spine Surgery Certified Physician
International University of Health and Welfare Atami Hospital Neurosurgery website
Yamagata University School of Medicine Graduated in 1989 Joined the University of Tokyo Neurosurgery Department
Doctor of Medicine (University of Tokyo "Analysis of the characteristics of head injuries caused by snowboarding and consideration of the mechanism of occurrence of intracranial injuries")
Dissertation abstract PhD original thesis
PhD original thesis![]() Abstract
Abstract
Qualifications/Licenses: Ordinary car license, Large motorcycle license, Kanji Test Level Pre-1
contact address
Department of Neurosurgery, International University of Health and Welfare Atami Hospital
13-1, Higashi-kaigan-cho, Atami, Shizuoka, Japan, 413-0012
Hospitals where I have worked
Fuji Brain Research Hospital, University of Tokyo Hospital, Kameda General Hospital, Saitama Medical University General Medical Center (Kawagoe), Suwa Chuo Hospital (Chief Neurosurgeon), Tokyo Welfare Pension Hospital (now JCHO Tokyo Shinjuku Medical Center, Chief of Neurosurgery), Teraoka Memorial Hospital (Director of Neurosurgery), Teikyo University Chiba General Medical Center (Lecturer of Neurosurgery, then Associate Professor of Stroke Center),Mitsui Memorial Hospital(Director of Neurosurgery).
Currently, I am engaged in neurosurgical treatment day and night as Professor at International University of Health and Welfare, Atami Hospital.
During my tenure at Mitsui Memorial Hospital (July 2012-March 2023), I introduced two surgical microscopes, a surgical navigation system, intraoperative ICG fluorescence diagnosis, intraoperative brain function and cranial nerve monitoring (transcranial MEP, SEP, ABR, VEP, lower cranial nerve monitor, facial stimulation, etc.) and established a system for cerebrovascular treatment, increasing the number of surgeries from 130 in 2012 to 305 in 2022.
.
As of March 2019, I was certified as a surgical technique instructor for stroke in Japan. Stroke surgical technical instructors are screened under the conditions of more than 100 aneurysm clipping surgeries and constant presentations at academic conferences and papers.As of April 2019, only 9.6% of neurosurgeon specialists are certified.
Nakaguchi was selected as an excellent doctor in the 5th edition of "the National Guide to Excellent Doctors and Hospitals" (Shufu to Seikatsusha, Japan).
Doctor of Doctors Network selected Nakaguchi as one of excellent specialist clinicians 2016-2019.
Papers written by Nakaguchi have been cited in numerous neurosurgery textbooks, as detailed in the "Papers and Presentations" section.
"Neurosurgery Revised 13th Edition (Kinpodo 2021)" p1128, 1129
"All about neurosurgical perioperative management 4th edition (Medical View, 2014)" p296, 300, p338
"Brain Tumor Therapeutics: Masao Matsutani (Kinpodo 2016)" p580-581, 604
"Archived Edition Diagnosis, Treatment and Surgery of Chronic Subdural Hematoma: Edited by Kentaro Mori (Medica Publishing 2017)" p74, 76, 123, 126, 131, 136
I wrote the reason why I became a neurosurgeon in the preface "Wisdom,Sentiment, Will" of Mitsui Memorial Hospital's public relations magazine "Living Together".
Wisdom, Sentiment, Will
neurosurgeon
Hiroshi Nakaguchi
My father was an otolaryngologist, and since I was a child, doctors were my closest occupation, but when I was in elementary school, I had a fear of doctors. When the blisters on my left palm became purulent and cellulitis due to overdoing horizontal bar exercise, I was incised in the hospital treatment room without anesthesia and the pain was so great that I couldn't say a word.
I had mild stomach pains and thought it was just a cold, but I was diagnosed with appendicitis and had surgery.
My impression at that time was that if I went to the hospital, I would be in pain.
What eased my fear of doctors was my interest in the natural sciences from a young age. When I was in 5th grade, I was fascinated by plankton, so my father bought me a microscope as a birthday present. When I was in the first year of junior high school, I read Tezuka Osamu's Phoenix, and I was moved by the hierarchical universe theory and the story of the birth of life. In high school, I was obsessed with Isaac Azimov's science essays. The more you know about science, the more detailed and complete the world seems, but the more mysterious it becomes. I decided to become a doctor because my interest in doctors outweighed my fear as I grew older. The impact of surgery when I was in elementary school led to my interest in surgeons, who cut the human body to directly observe and treat the causes of illness. I have a particular interest in surgery.
Neurosurgeons require not only the strict morals and ethics of a medical doctor, but also special professional ethics to deal with stroke care and emergency surgery day and night. From Shichihei Yamamoto's "The Spirit of Japanese Capitalism", Japan's unique capitalist morality, which began with Shozo Suzuki in the Edo period and was completed by Baigan Ishida's Sekimon Shingaku = Daily labor itself is a Buddhist training, Knowing that there is a lineage of Japan's unique occupational ethics that believes that liberation (= mental well-being) can only be obtained through work, I feel that it matches my view of work as a neurosurgeon who does not seek compensation or reward alone.
After graduating from Yamagata University School of Medicine, starting with Fuji Brain Research Hospital, University of Tokyo Hospital, Kameda General Hospital, Saitama Medical University General Medical Center, Suwa Central Hospital, Tokyo Welfare Pension Hospital, Teraoka Memorial Hospital, Teikyo University Chiba General Medical Center I have learned a lot about brain surgery. What I thought was particularly important through actual clinical practice is that neurosurgical treatment cannot be done without community medicine, and that teamwork inside and outside the organization is more important than anything else in the harshness of neurosurgery. As an instructor, it is important not only to perform surgery and treatment, but also to bring people together.
Reflecting on this, I can say that the various experiences I have encountered in my life have been inevitable for my current work. I would like to continue my life as a neurosurgeon, never forgetting the frontier spirit of my student days of wanting to explore the mysteries of the world through the inside of the human body, which is the building block of the universe, and the causes and treatment of diseases.
[Surgery experience]
From here, I will explain the surgeries I have performed, with photos.
Prior to that, I would like to state my basic thoughts on cerebral aneurysms (unruptured + ruptured).
Unruptured brain aneurysm
An unruptured cerebral aneurysm may be found during a brain checkup, or an aneurysm may be found incidentally when a brain MRA is taken for a headache, etc.
At the age of 50, 4% of men, 6% of women, and 7-8% of people in their 70s have an unruptured cerebral aneurysm.When an unruptured cerebral aneurysm was discovered, I explained to the patient as follows.
“There is a 0.95% chance of a cerebral aneurysm rupturing in one year, or even a subarachnoid hemorrhage. In order to avoid the 0.95%, it is important not to develop arteriosclerosis and to live a calm life.
If you have high blood pressure, diabetes, or hyperlipidemia, get proper treatment, exercise moderately, eat well, and drink water in moderation.If the cerebral aneurysm is 6 mm or more in size, or if the tip of the aneurysm protrudes and ruptures easily, it is thought that subarachnoid hemorrhage is likely to occur.
If a cerebral aneurysm ruptures and causes subarachnoid hemorrhage, it is said that 30 to 40% will die even if treated. Craniotomy aneurysm clipping) and endovascular surgery (cerebral aneurysm coil embolization) should be seriously considered.
However, it is said that there are 3 to 6% of surgical complications (1 to 2% for severe disability) even if the surgery is performed carefully.
When performing surgery, we do our best to perform surgery with few surgical complications. ”
Ruptured brain aneurysm
If a cerebral aneurysm ruptures and causes subarachnoid hemorrhage, it is said that 15% of people will die on the spot, but if they survive, they will be transported to the hospital by ambulance.
If a cerebral aneurysm reruptures, the mortality rate rises sharply, so an emergency cerebral angiography test is performed to accurately determine the location of the aneurysm, and as a general rule, within 24 hours or less, clipping to stop rebleeding within 48 hours. Surgery (or endovascular coil embolization) is performed (however, if the patient's condition is too bad, surgery itself may not be possible).
After surgery, we aim to return to society by appropriately treating cerebral vasospasm and hydrocephalus.
With a few exceptions, aneurysms can occur in 6 sites, and the surgical approach for each site is almost established.
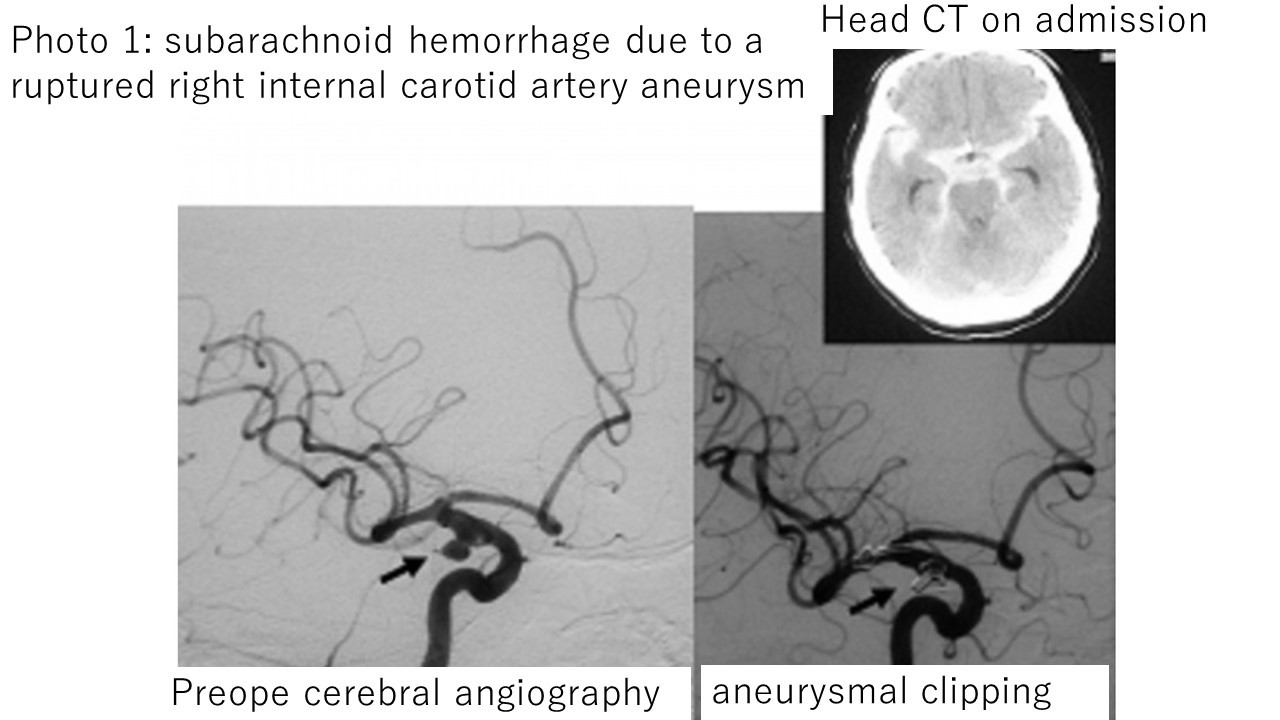
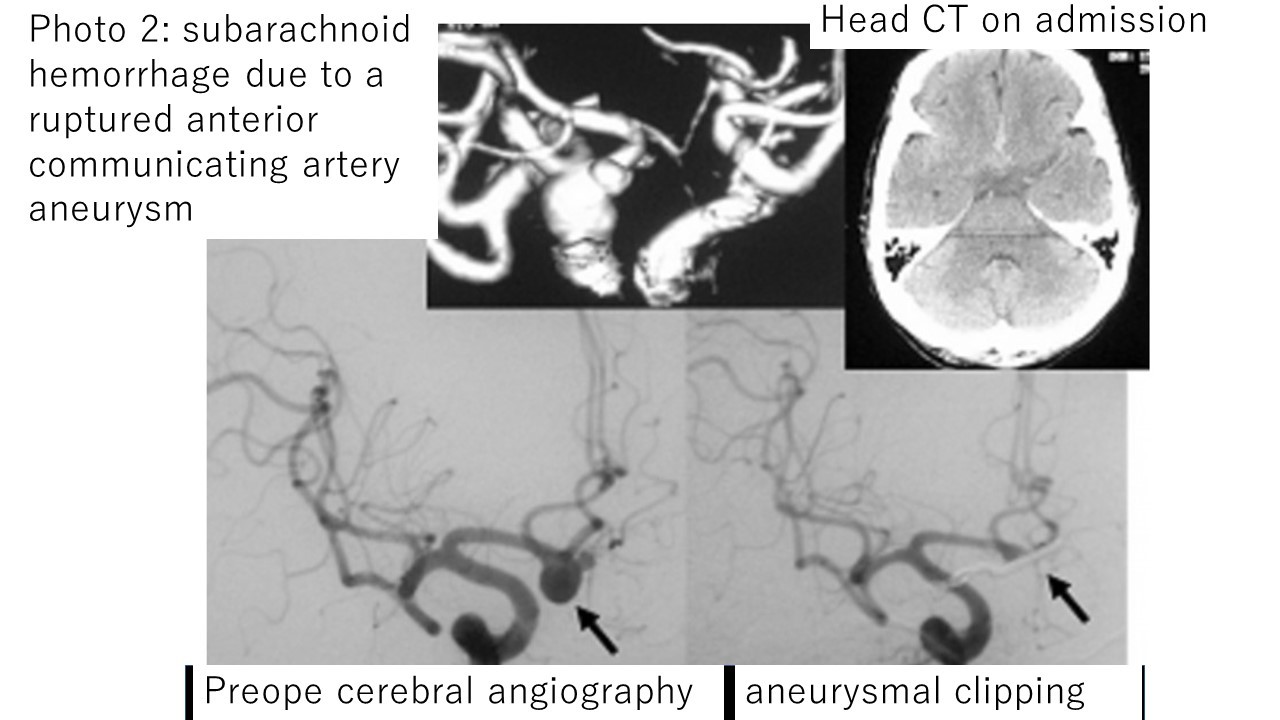
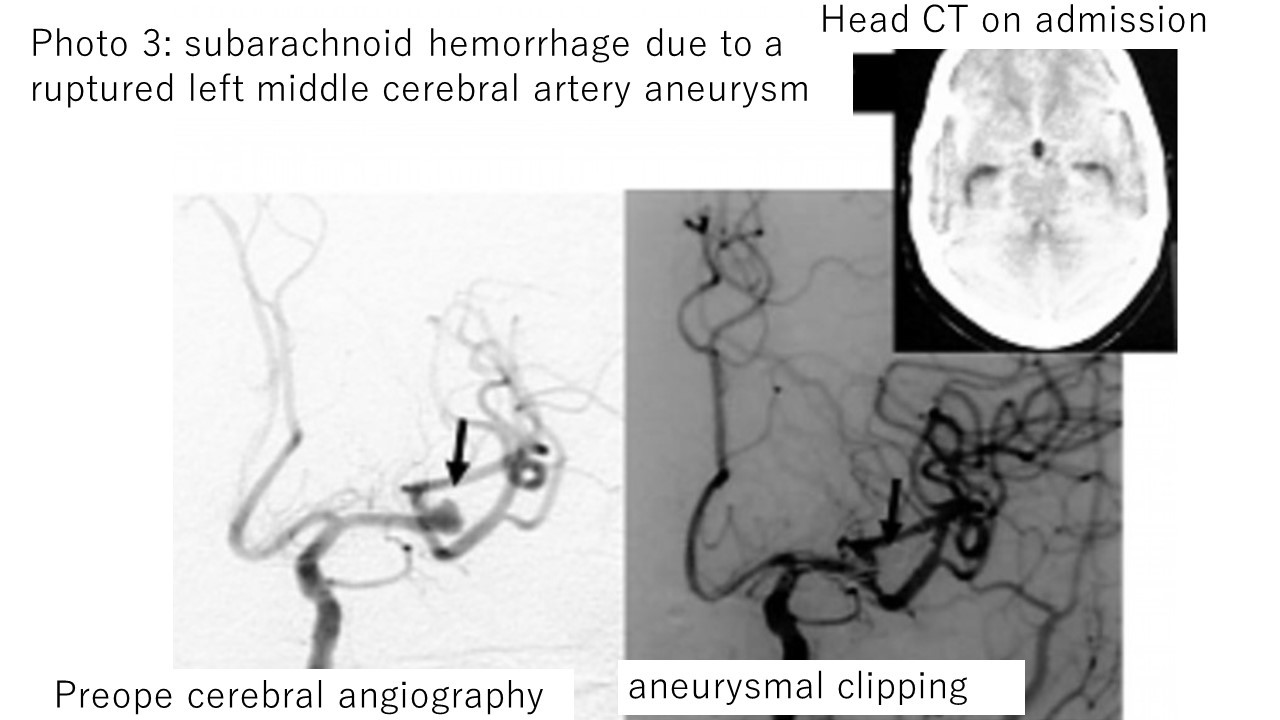
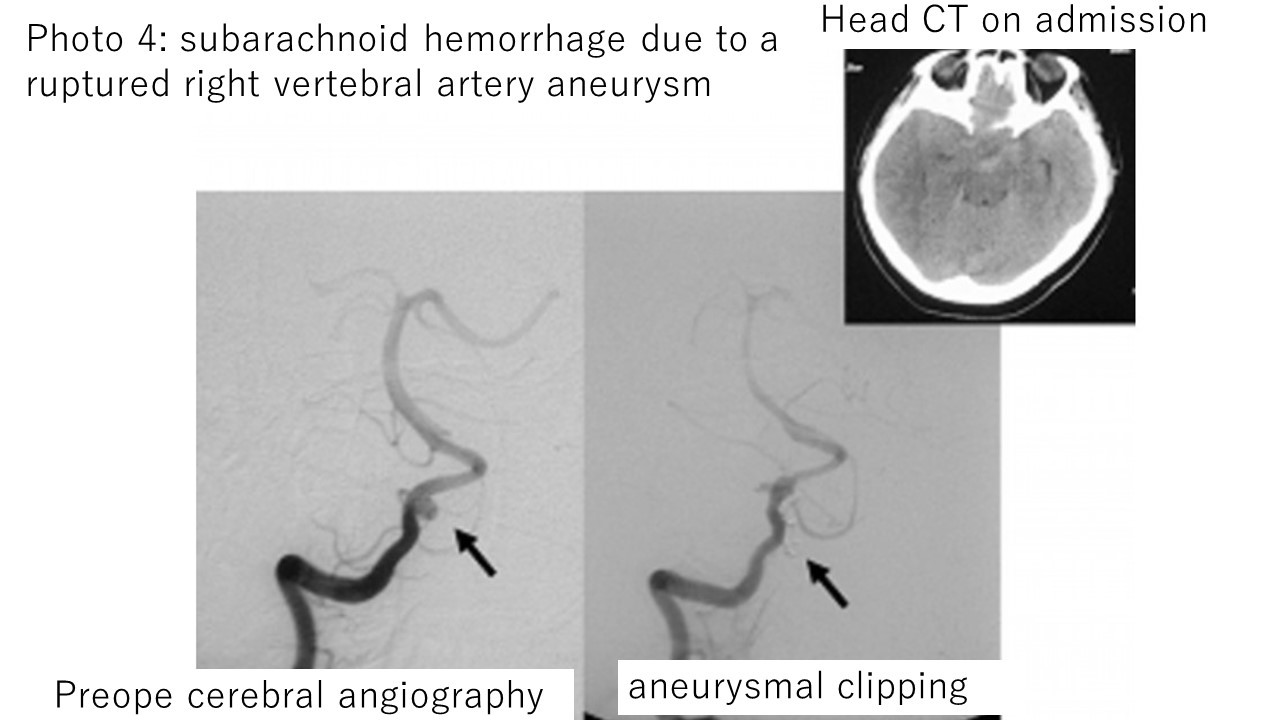
Photographs 1 to 4 explain the clipping surgery for aneurysms in four different sites that I actually performed for subarachnoid hemorrhage (all of these cases were fortunately free from symptoms and left the hospital on their own).
Photo 1: Clipping surgery for subarachnoid hemorrhage (right internal carotid aneurysm).
The image on the left is a cerebral angiography before surgery, and the image on the right is a cerebral angiography after surgery.
Photo 2: Clipping surgery for subarachnoid hemorrhage (anterior communicating artery aneurysm).
The image on the left is a cerebral angiography before surgery, and the image on the right is a cerebral angiography after surgery.
Photo 3: Clipping surgery for subarachnoid hemorrhage (left middle cerebral aneurysm rupture).
The image on the left is a cerebral angiography before surgery, and the image on the right is a cerebral angiography after surgery.
Photo 4: Clipping surgery for subarachnoid hemorrhage (right vertebral aneurysm).
The image on the left is a cerebral angiography before surgery, and the image on the right is a cerebral angiography after surgery.
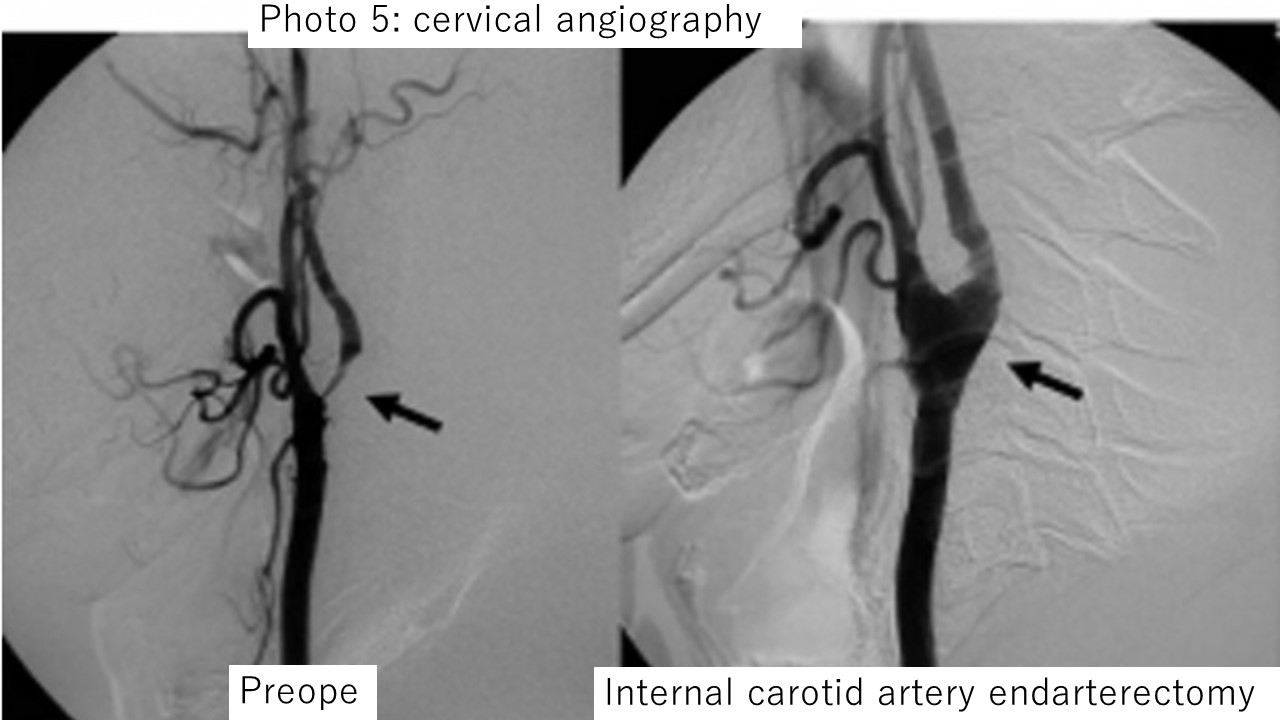
Internal carotid artery endarterectomy

The internal carotid artery, which supplies oxygen and nutrients to the brain through the neck, is always under high pressure, so it is prone to arteriosclerosis.If severe stenosis is found on the internal carotid artery, a surgical procedure called internal carotid artery endarterectomy, which removes the narrowed portion of the arterial wall, can prevent cerebral infarction.
Photo 5: Left internal carotid endarterectomy for severe left internal carotid artery stenosis.The left is the preoperative cerebral angiography, and the right is the postoperative cerebral angiography.It can be seen that the internal carotid artery stenosis has expanded significantly after surgery.The patient was discharged home with no symptoms other than the original symptom (mild right paralysis).
Recently, the development of cerebral endovascular surgery tools has been remarkable, and the method of correcting stenosis by inserting a stent in the carotid artery has become common.
Superficial temporal artery-middle cerebral artery anastomosis
If the blood vessels in the brain are narrowed or clogged, it may be effective to reconstruct the arteries using the blood vessels under the skin (however, this surgery is only for those who meet strict indication criteria).
Even children in the lower grades of elementary school can develop a disease in which the arteries of the brain gradually narrow (a disease called moyamoya disease, which is common among Japanese people).
In this case as well, surgery is performed to improve blood flow to the brain by connecting the subcutaneous artery in front of the ear (called the superficial temporal artery) to blood vessels in the brain.
Photo 6: Right superficial temporal artery-middle cerebral artery anastomosis for right internal carotid artery occlusion.
Cerebral angiography before surgery (left) and cerebral angiography after surgery (right) confirm good blood flow from the extracranial artery (superficial temporal artery) to the intracranial artery (middle cerebral artery) (→).
The patient was asymptomatic and discharged on his own.
Photo 7: Cerebral blood flow examination (SPECT) in Photo 6.
Left is before surgery, right is after surgery.
Postoperative SPECT showed a marked increase in blood flow in the right frontal lobe (→).
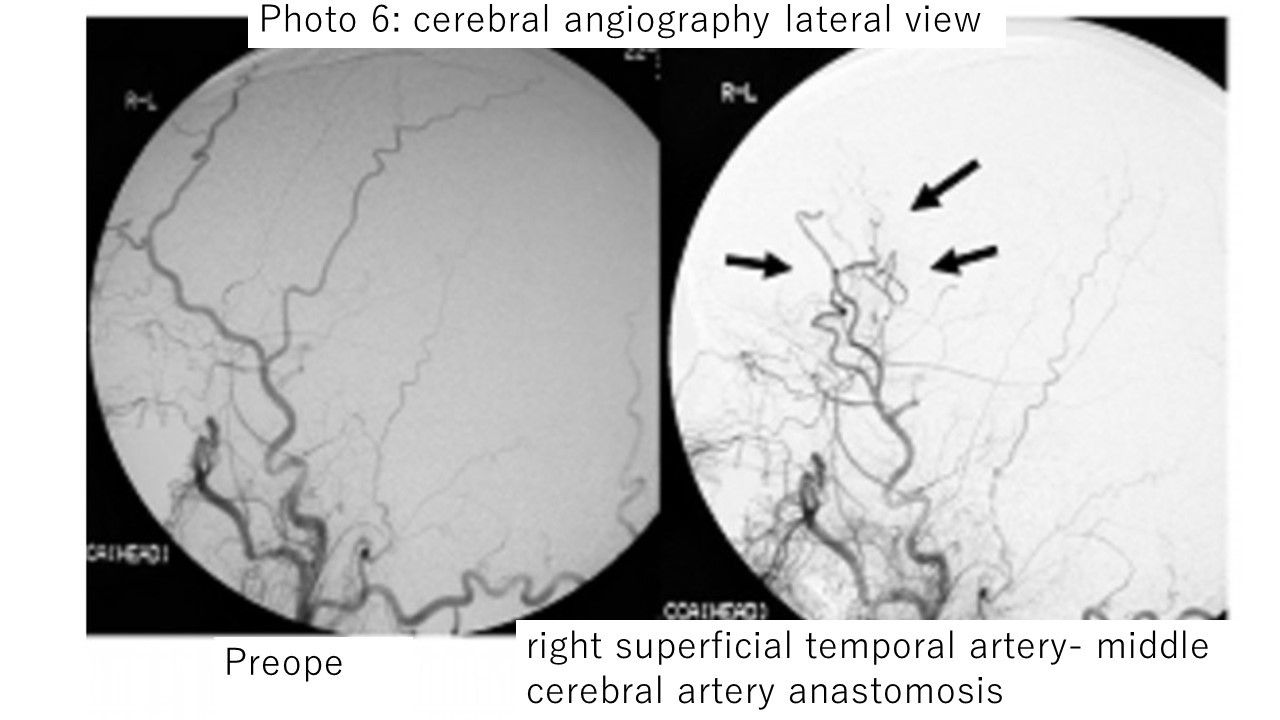
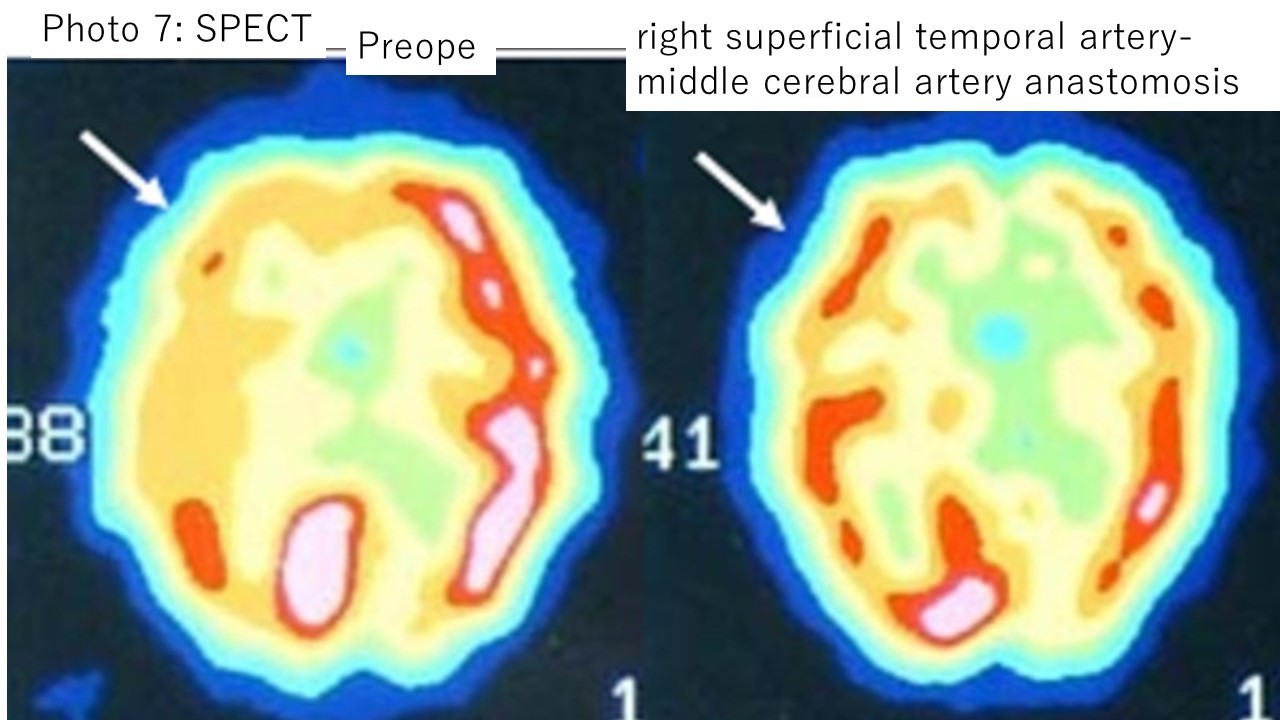
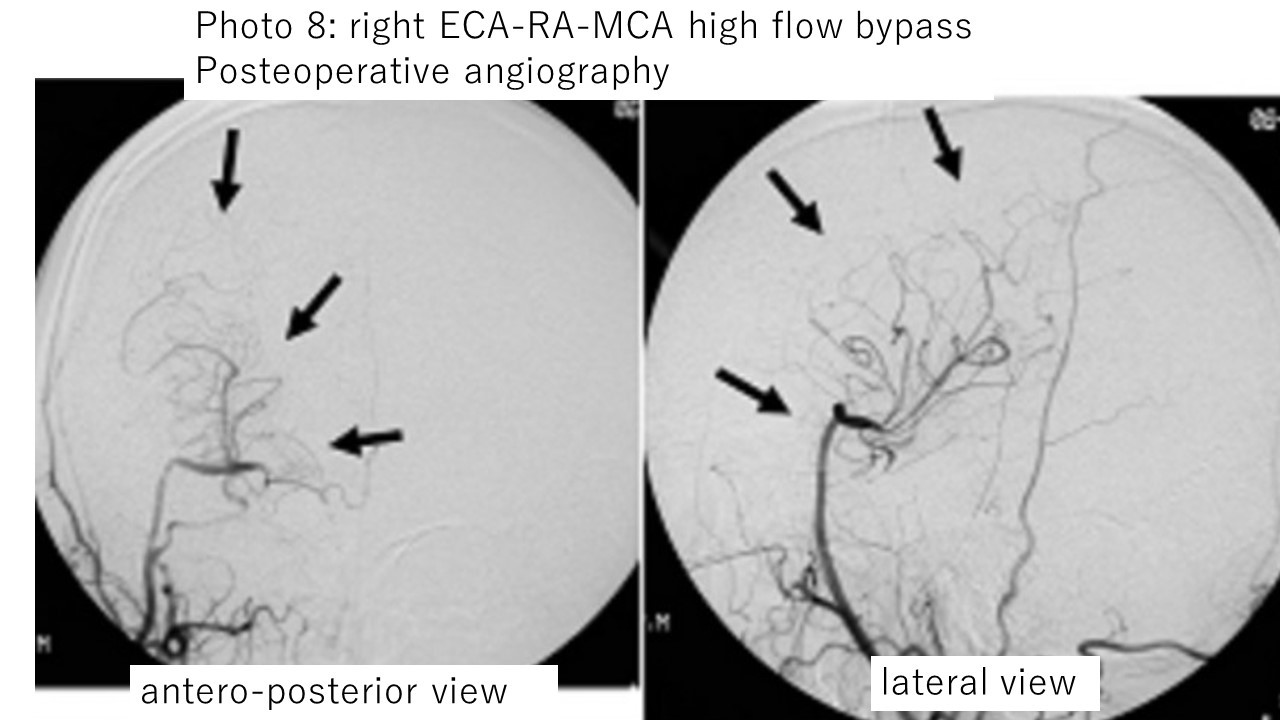
Photo 8: Postoperative cerebral angiography of extracranial-vascular intracranial vascular bypass surgery using the left radial artery (right common carotid artery-radial artery graft-right middle cerebral artery anastomosis) for right internal carotid artery occlusion.
Good blood flow is confirmed through the bypass into the skull (→).
The patient was asymptomatic and discharged on his own.
Cervical spine surgery
Diseases of the cervical spine include intervertebral disc herniation, cervical spondylosis, posterior longitudinal ligament ossification, and atlantoaxial subluxation.
For moderate neurological symptoms (such as numbness in the hands), surgery can prevent the symptoms from progressing.
However, if the limbs are already paralyzed before the operation, it is difficult to recover completely even with surgery, so surgery must be considered before severe paralysis occurs.
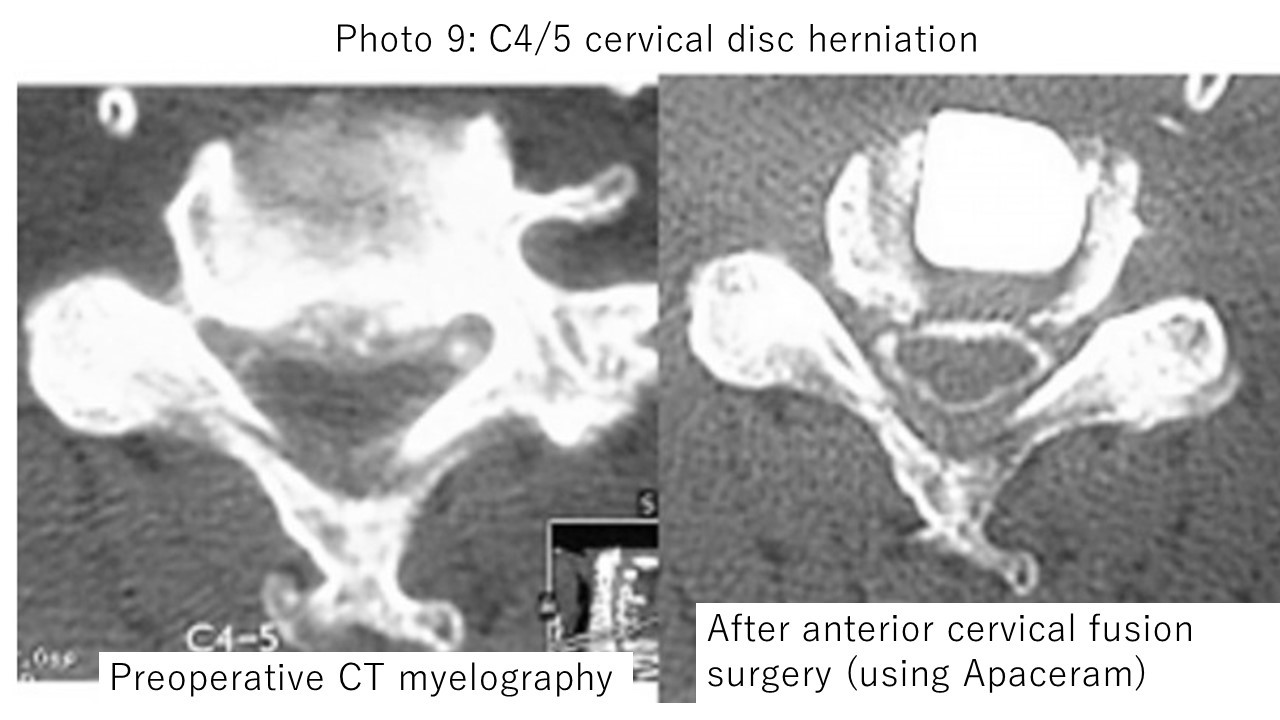
Photo 9:Gait disturbance and finger numbness were diagnosed as caused by cervical disc herniation.The spinal cord is compressed at the 4th-5th cervical vertebrae in myelography examination before surgery, and deformation is seen.
Postoperative myelography showed the spinal cord was not compressed in the surgical area.
The patient's preoperative symptoms improved and he was discharged home.
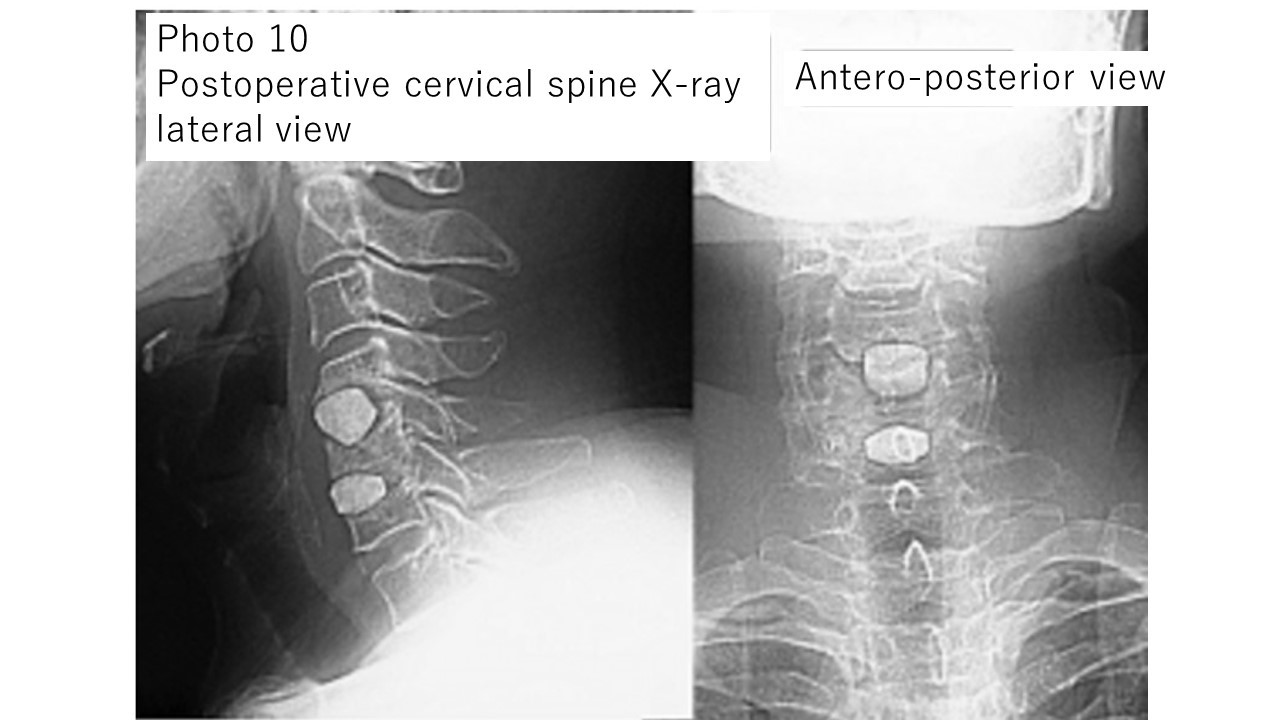
Photo 10: Plain X-ray image of the cervical spine after surgery for the patient in Photo 9.
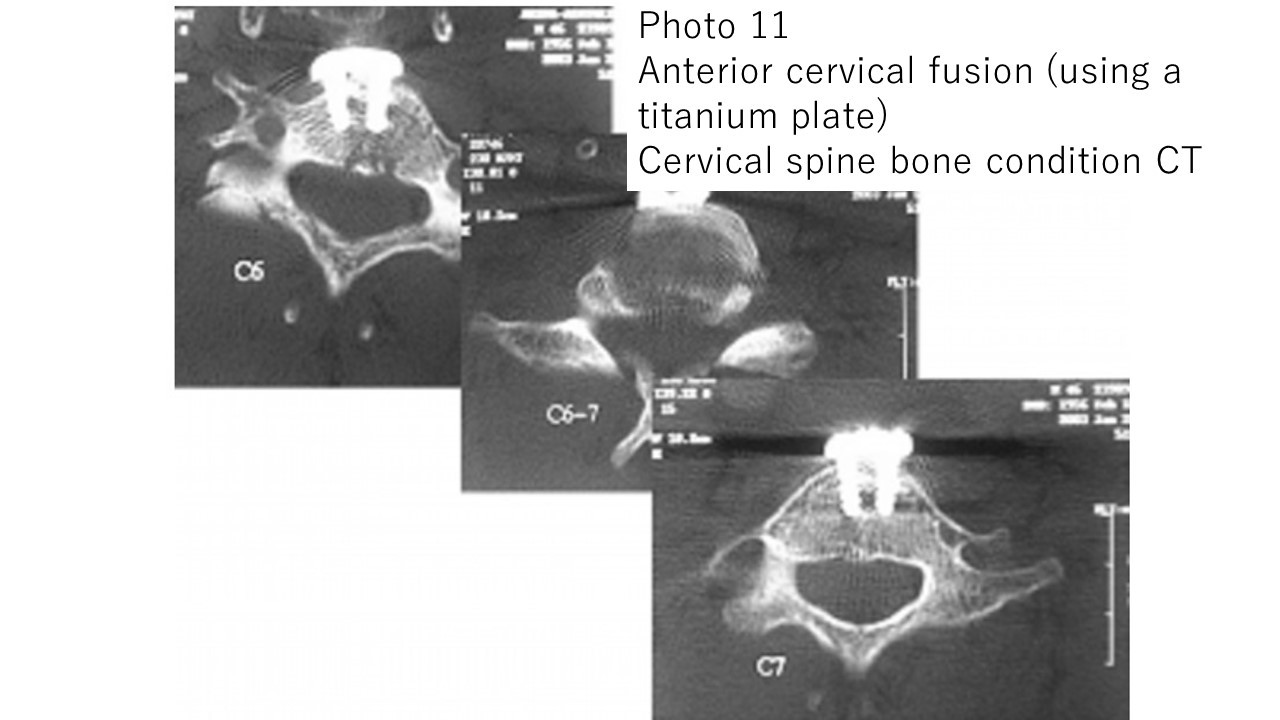
Photo 11: Anterior fusion surgery (using a titanium plate) was performed for a cervical fracture (traffic accident).
Postoperative CT scan of the cervical spine. The titanium plate is firmly fixed with four screws.
The patient was discharged home on foot 2 weeks after surgery.
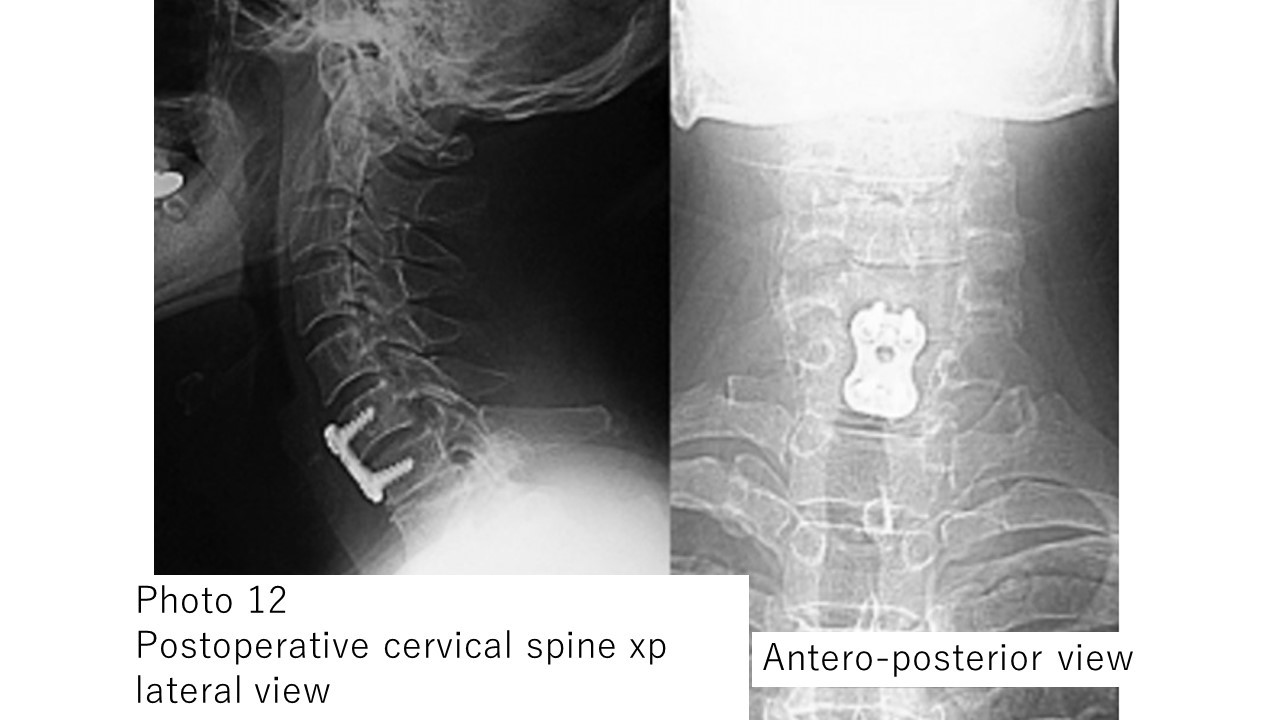
Photo 12: Plain X-ray image of the cervical spine after surgery for the patient in Photo 11
。
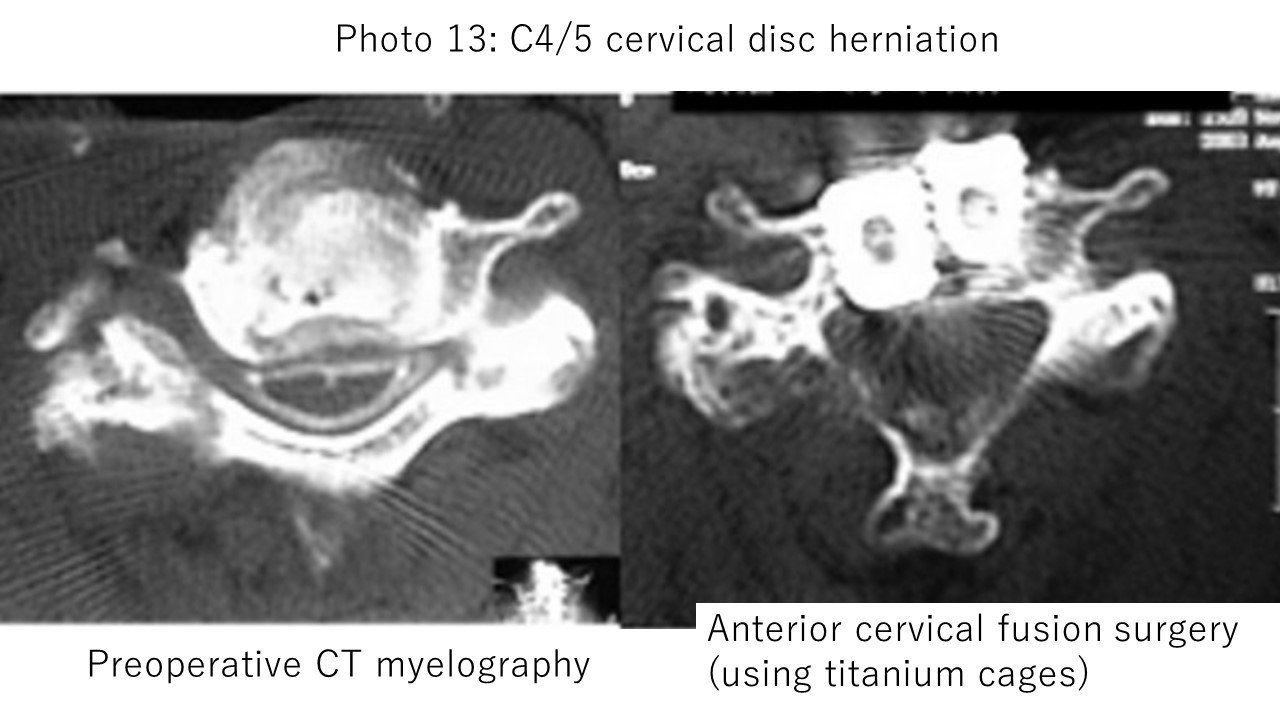
Photo 13: Due to cervical disc herniation, there was gait disturbance and numbness in the fingers, and cervical spine anterior fusion surgery (using a titanium cage) was performed.
Postoperative cervical spine CT examination showed that the spinal cord was not compressed in the operated area.
The patient's preoperative symptoms improved and he was discharged home. This surgery is a relatively new technique in which a titanium screw is inserted in place of the removed intervertebral disc to fix it.
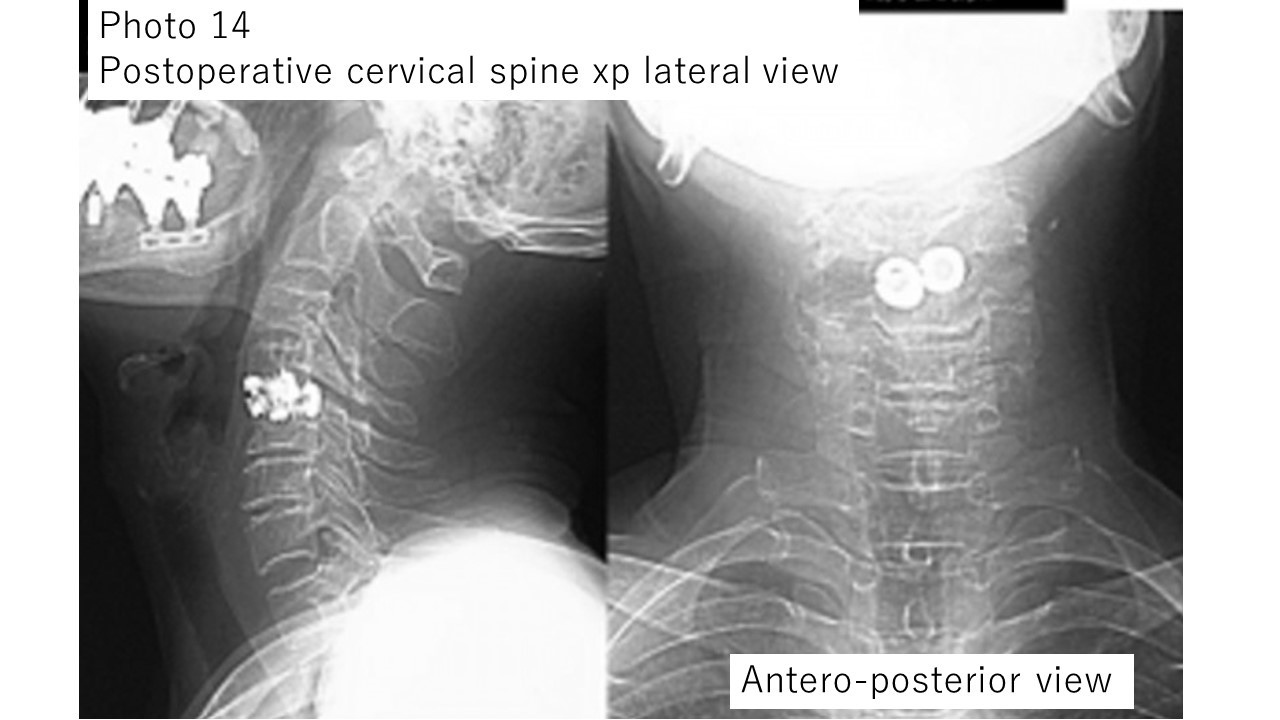
The patient became ambulatory early after surgery and was discharged home 2 weeks after surgery.Photo 14: Plain X-ray image of the cervical spine after surgery for the patient in Photo 13.
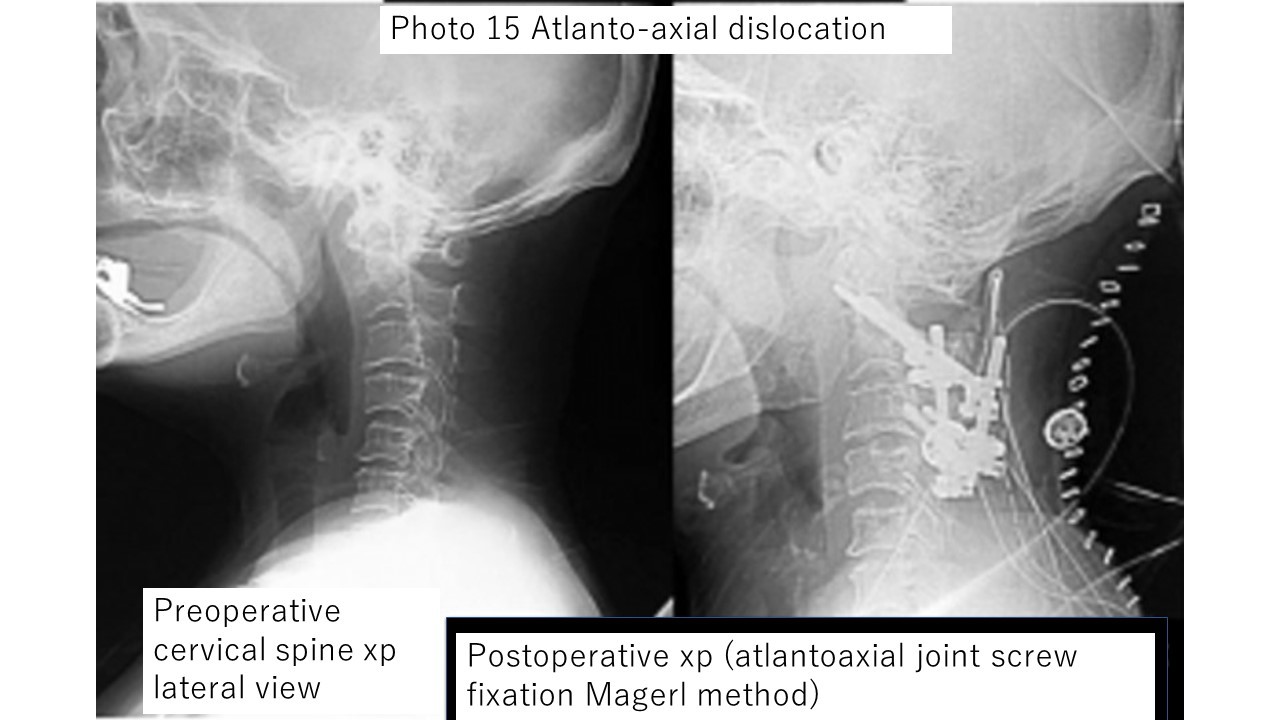
Photo 15: Atlantoaxial subluxation is a terrifying condition in which the first cervical vertebra (called the atlas) and the second cervical vertebra (called the axis) are misaligned, and in severe cases breathing may stop.
The image on the left is before surgery, and the image on the right is after surgery.
The atlas and axis are firmly fixed with large screws.
The patient was discharged from the hospital on foot with no new symptoms after surgery.
Intracerebral hematoma removal
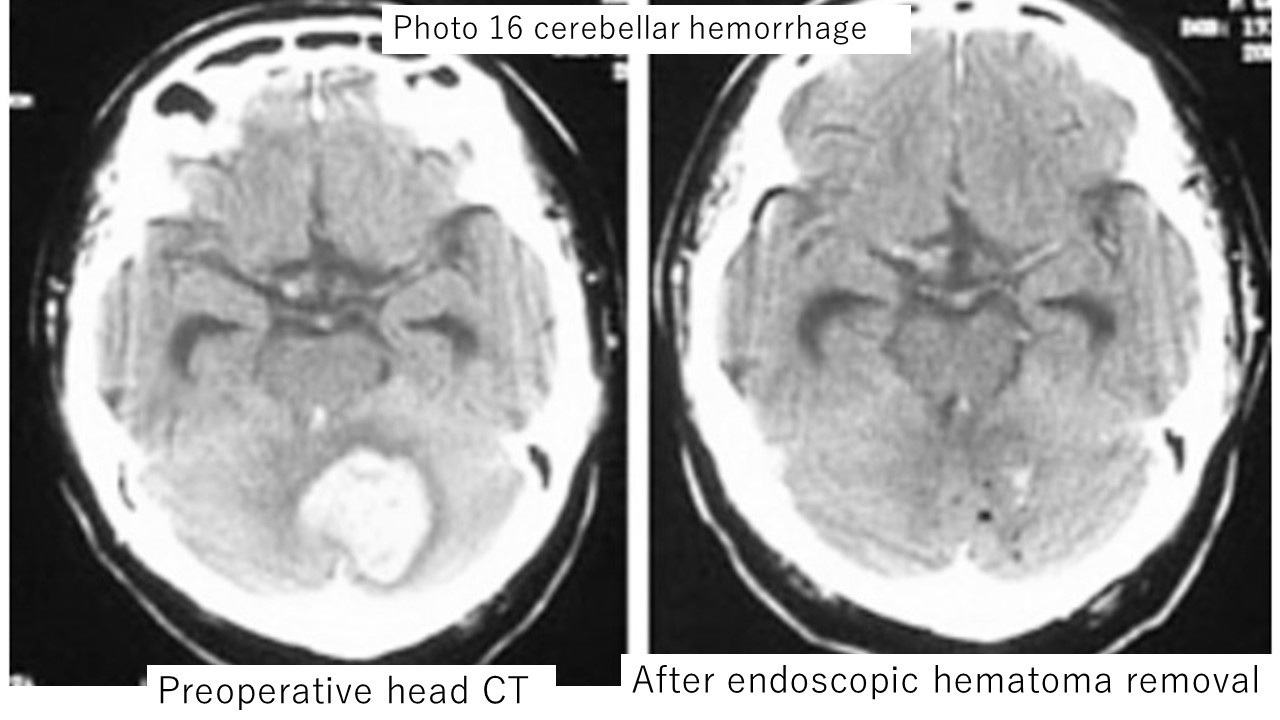
Endoscopic hematoma removal may be performed for some intracerebral hemorrhages in the elderly or those with systemic complications.
The operation takes 1 to 2 hours and is less invasive to the patient, but craniotomy is more effective when the amount of bleeding is large and the swelling of the brain is severe.
Photo 16: Endoscopic hematoma removal for cerebellar hemorrhage. The left is a CT image at admission, and the right is a CT image after surgery. Almost all hematomas have been removed.
brain tumor
I perform resection of a wide variety of intracranial tumors such as meningiomas, malignant tumors (metastatic brain tumors, gliomas, etc.), acoustic neuroma, and accurate pathological diagnosis, followed by radiotherapy and chemotherapy.
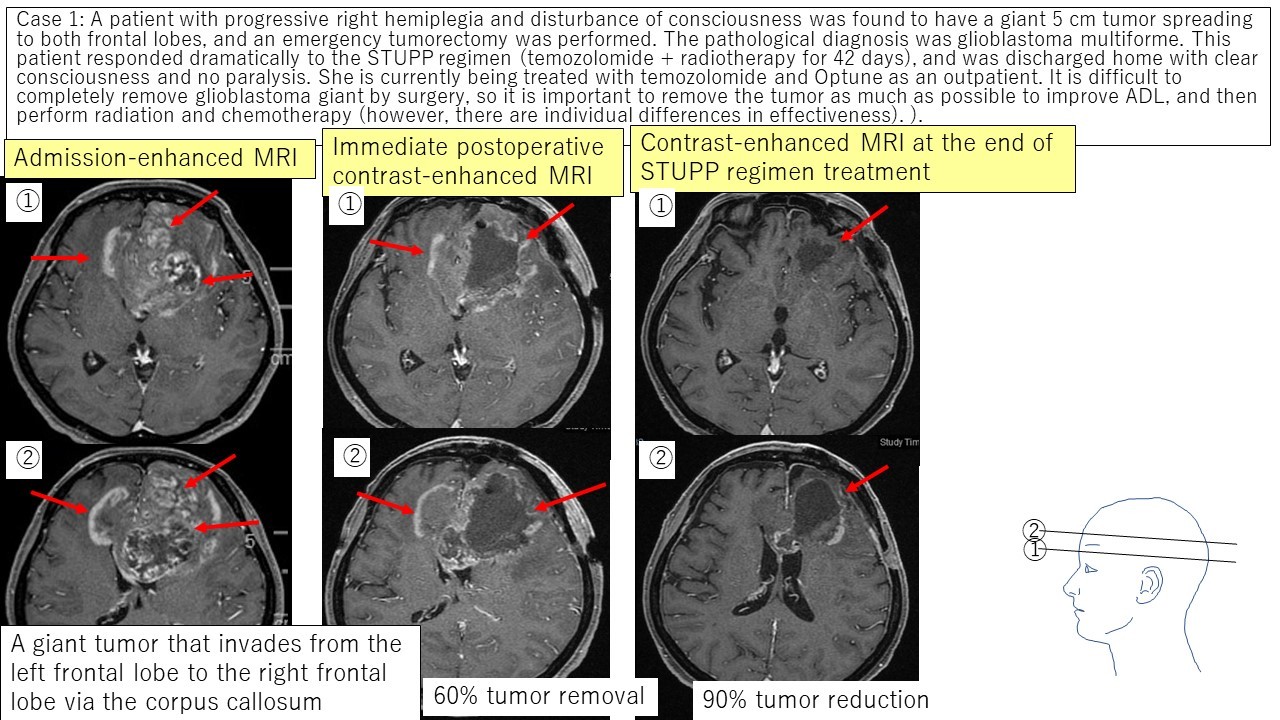
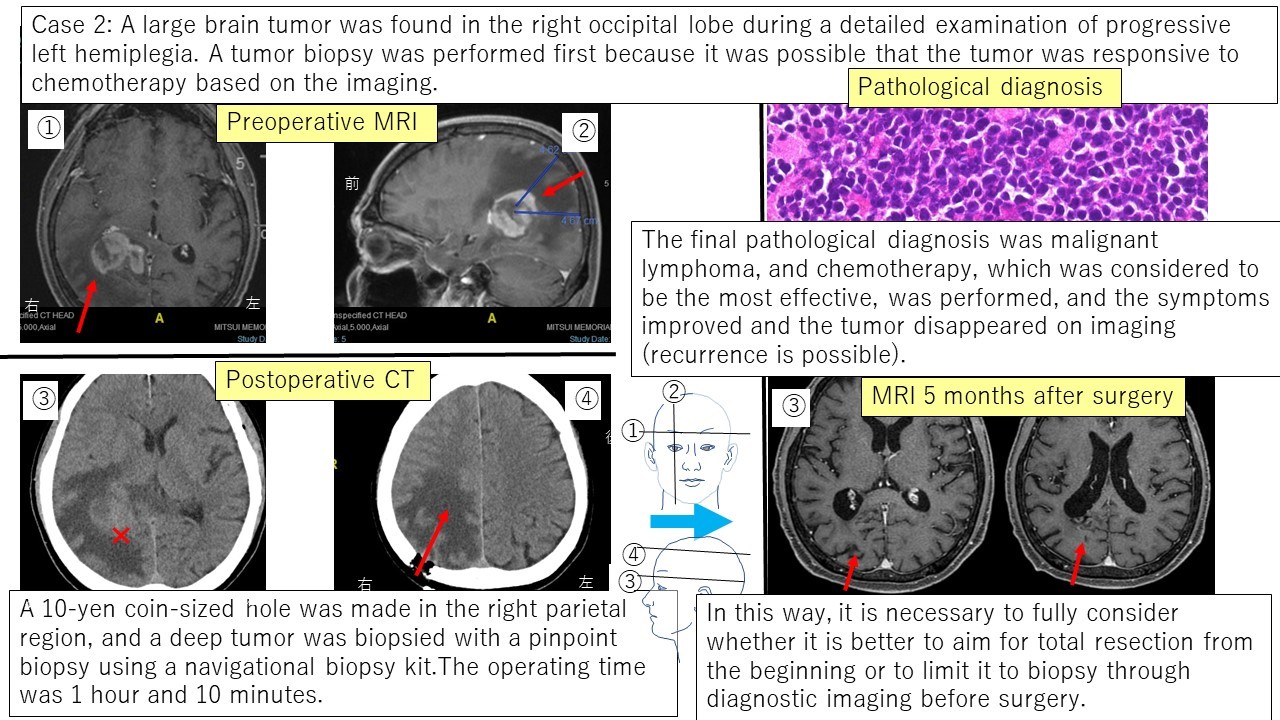
Since brain tumors grow in the closed space of the skull, it is necessary to pay close attention to adhesions to the surrounding brain and treatment of infiltration sites.To perform a safe and reliable brain tumorectomy,(1) Consider the safest and easiest approach to surgery before surgery,(2) To know exactly where the tumor is currently being removed during surgery,(3) At the time of tumor resection, efforts should be made to preserve the function of the cerebral blood vessels and cranial nerves within or in contact with the tumor.are particularly important.After surgery, it is important to (4) examine the excised tumor by pathology, and carefully monitor the progress of tumors that can be predicted to recur easily.Basically, if these four points are suppressed, surgery can be safely performed on any tumor at any site (although it is important to set up different strategies for tumors with different characteristics, tumor removal The concept of the operation itself is the same.)
From that point of view, I have devised a variety of methods for craniotomy to remove tumors, and have performed complete resections while preserving function, even for tumors that are difficult to remove.Due to space limitations, I would like to explain the contents of my papers and conference presentations so far in topics.
Regarding①,
⇒ 「Knowing about the treatment of brain tumors Part 1 Ingenuity of craniotomy tumor resection (using the MRI FLAIR method)
「Knowing about the treatment of brain tumors Part 1 Ingenuity of craniotomy tumor resection (using the MRI FLAIR method)
と Knowing the Treatment of Brain Tumors Part 3: Ingenuity of Craniotomy Tumor Resection (Surgery Using the Cerebral sulcus)
Knowing the Treatment of Brain Tumors Part 3: Ingenuity of Craniotomy Tumor Resection (Surgery Using the Cerebral sulcus)
Regarding ②③,
⇒ Knowing the Treatment of Brain Tumors Part 2 Ingenuity in Craniotomy Tumor Resection (Intraoperative Navigation and Intraoperative Monitoring)
Knowing the Treatment of Brain Tumors Part 2 Ingenuity in Craniotomy Tumor Resection (Intraoperative Navigation and Intraoperative Monitoring)
Regarding ④,
I would like to show you the progress of brain tumor patients who actually underwent surgery at Mitsui Memorial Hospital recently (all performed by Nakaguchi).
malignant brain tumor
① Glioblastoma multiforme Case 1
② Malignant lymphoma Case 2
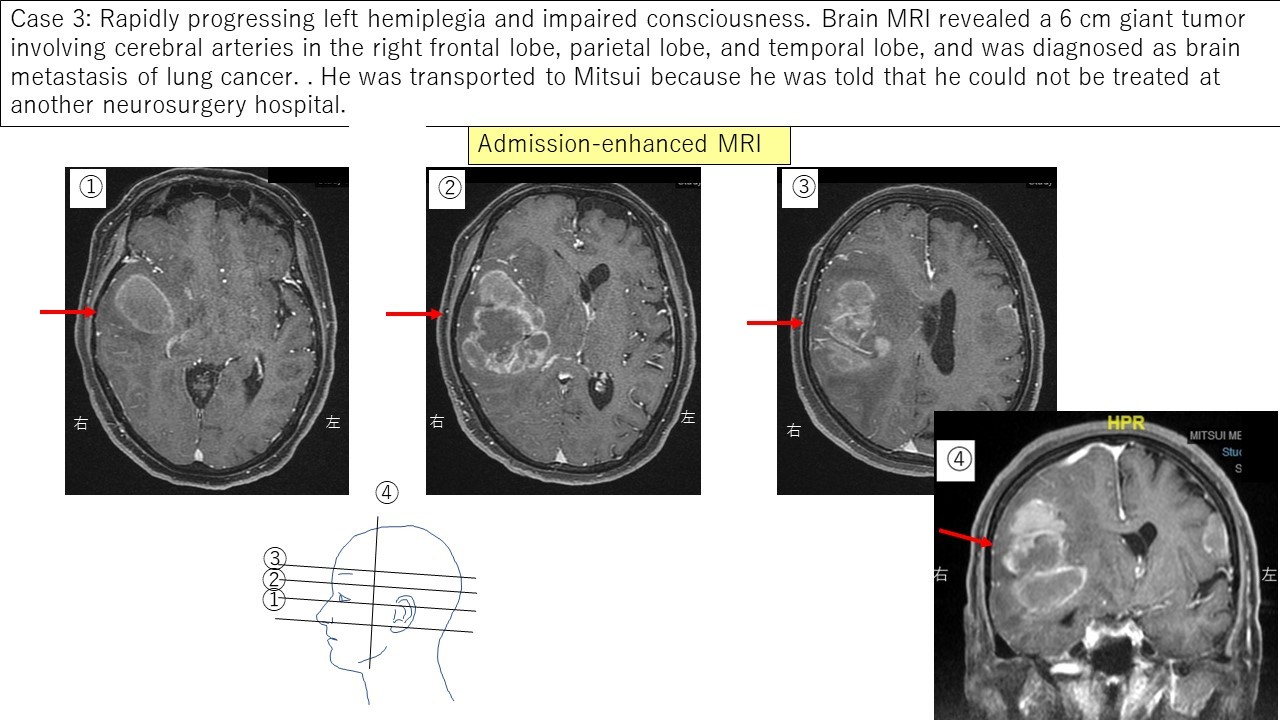
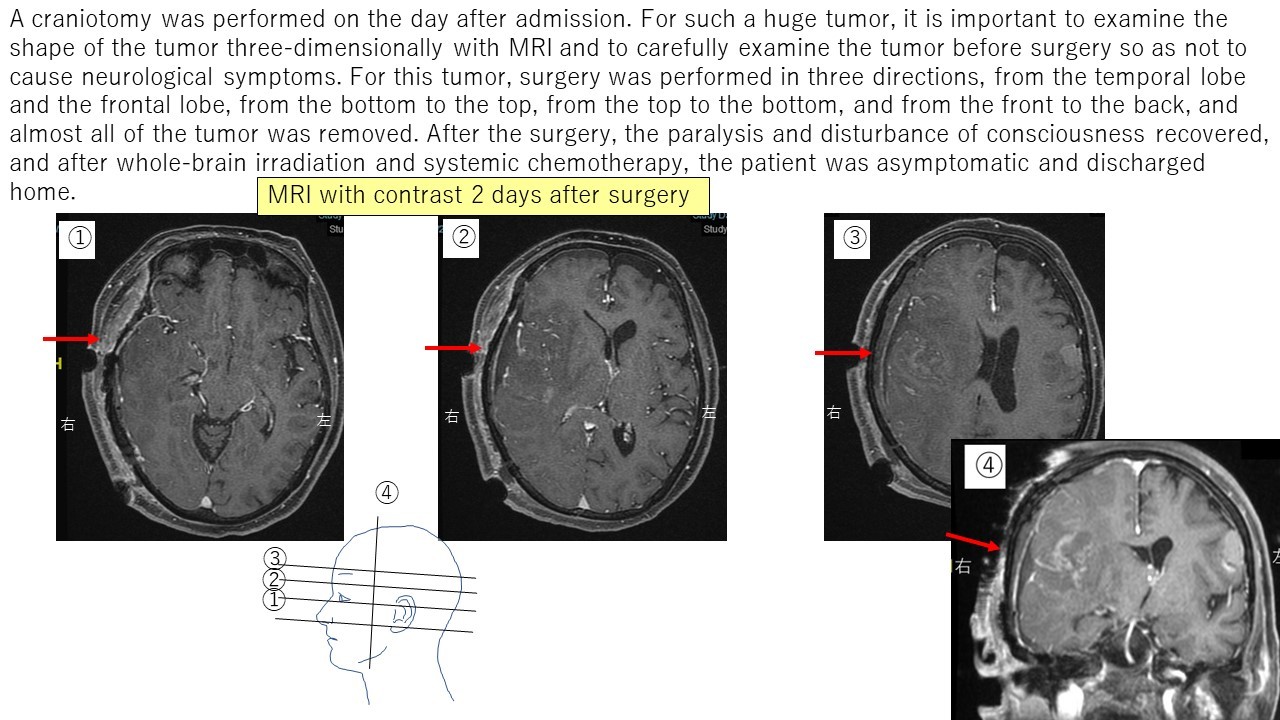
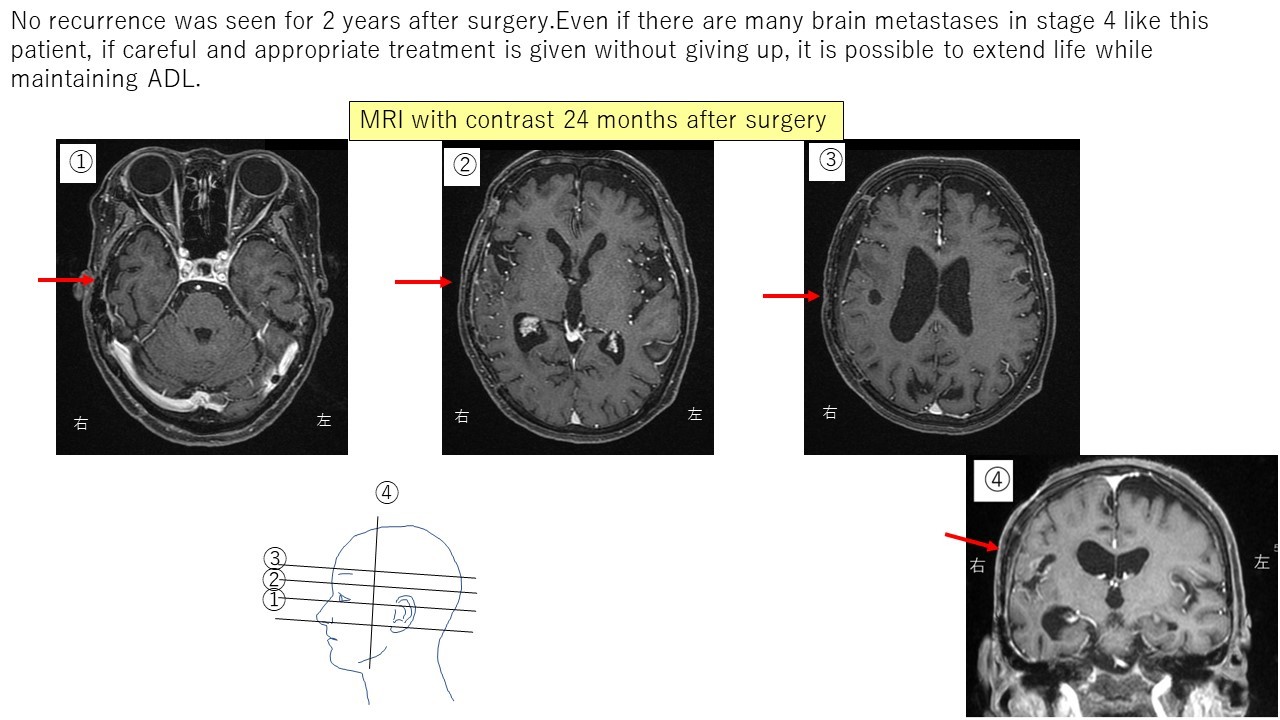
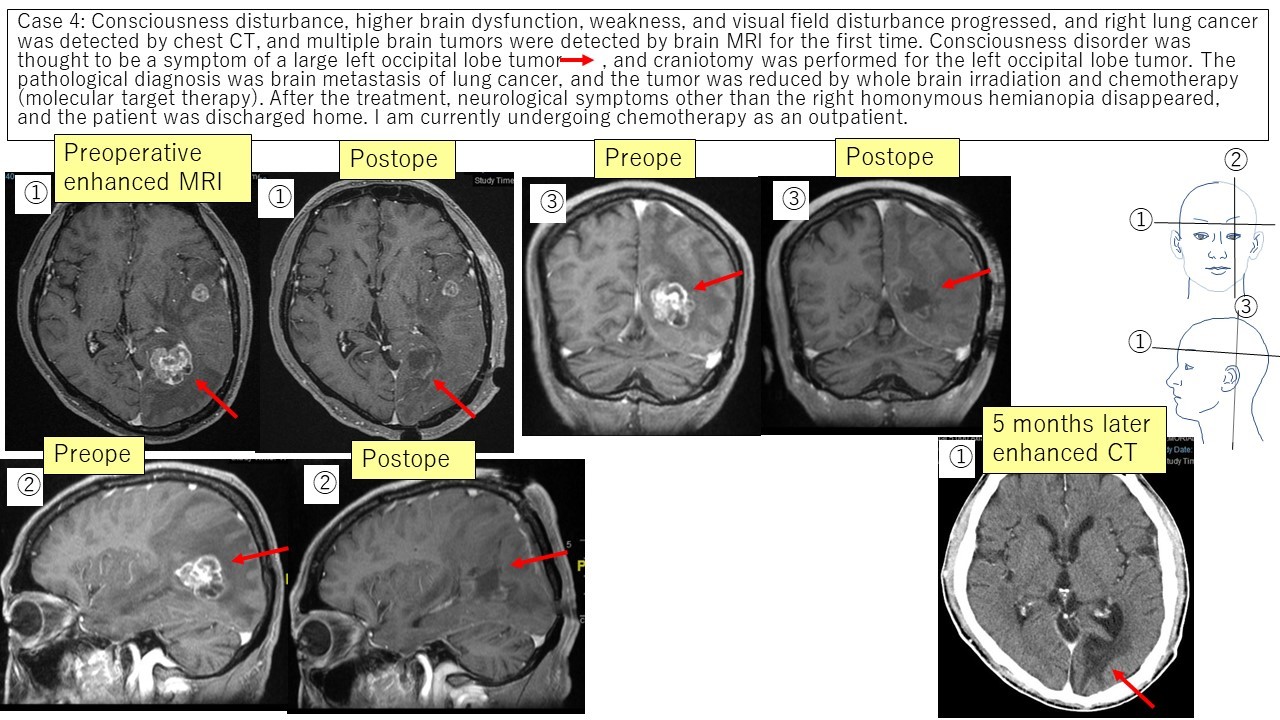
③ Metastatic brain tumor Case 3 Case 4
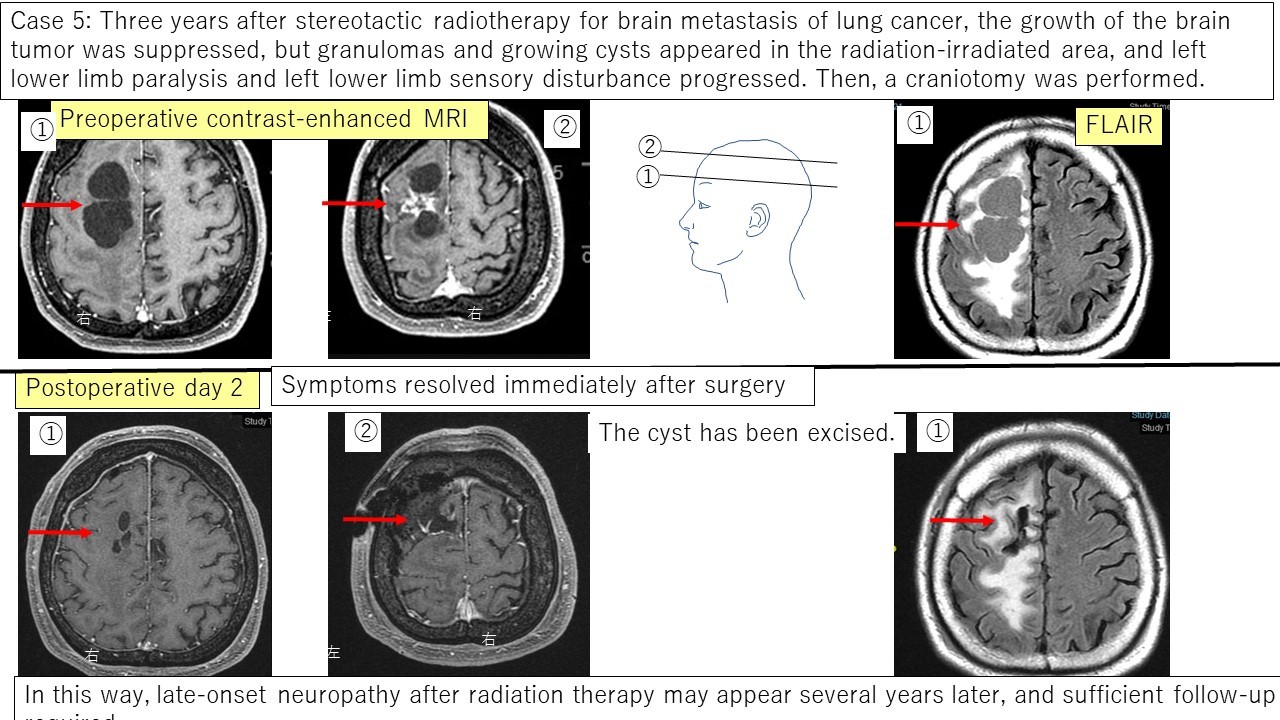
④ Delayed radiation necrosis Case 5
benign tumor
① Meningioma
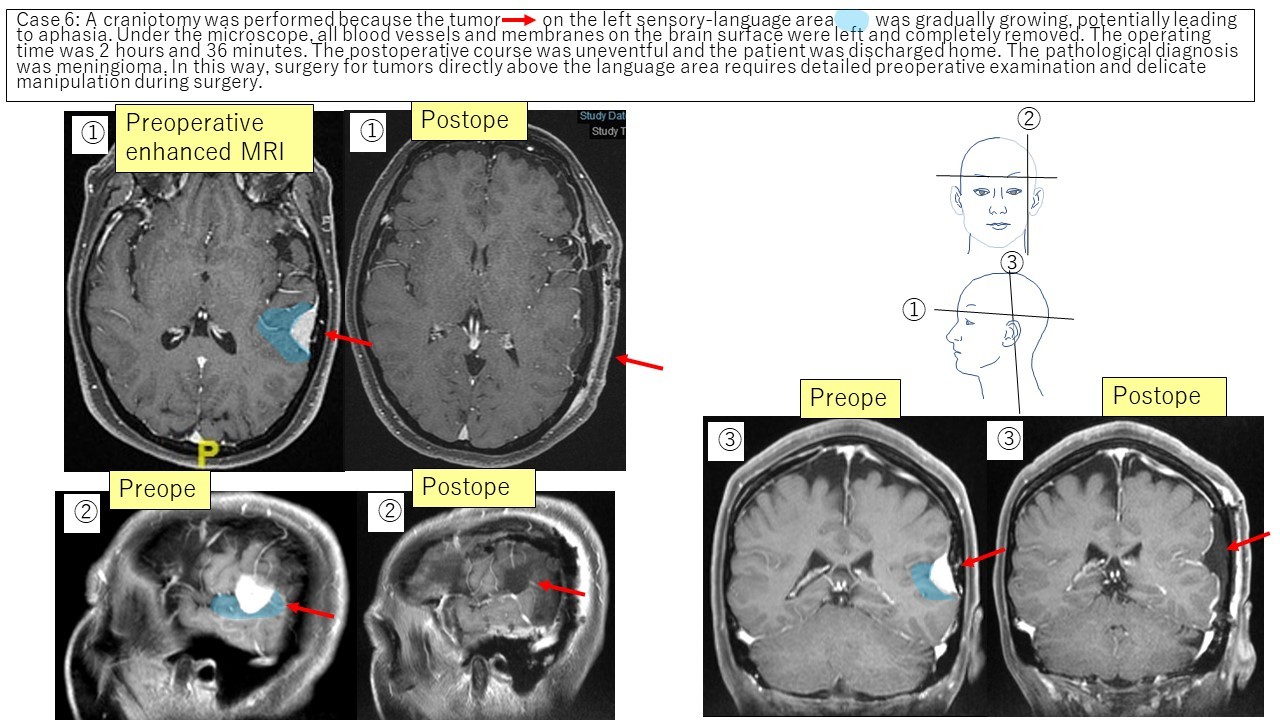
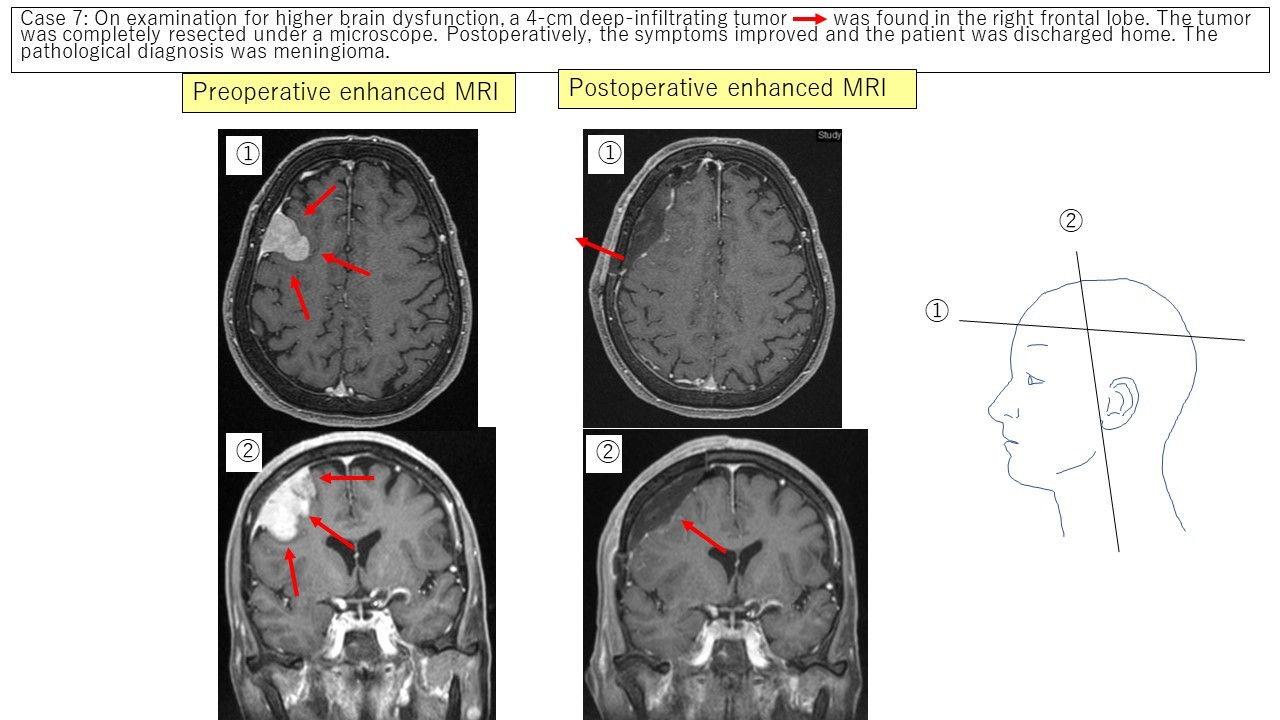
Vault meningioma Case 6 Case 7
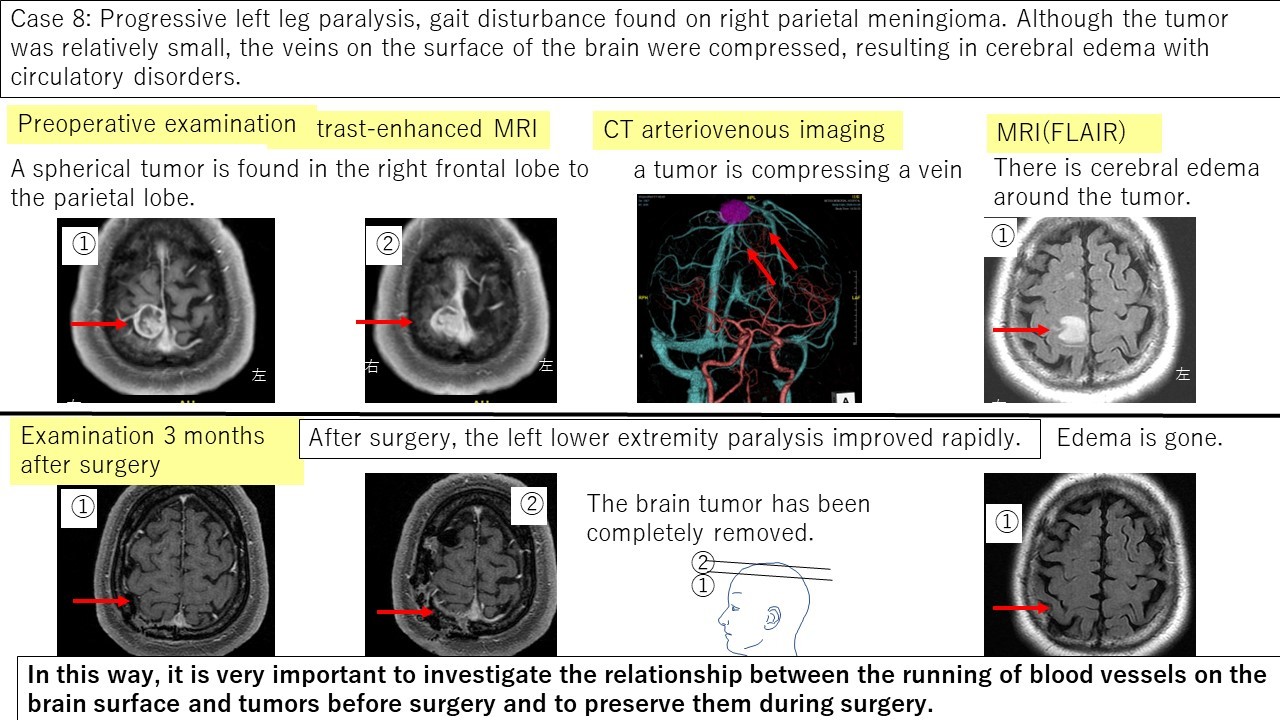
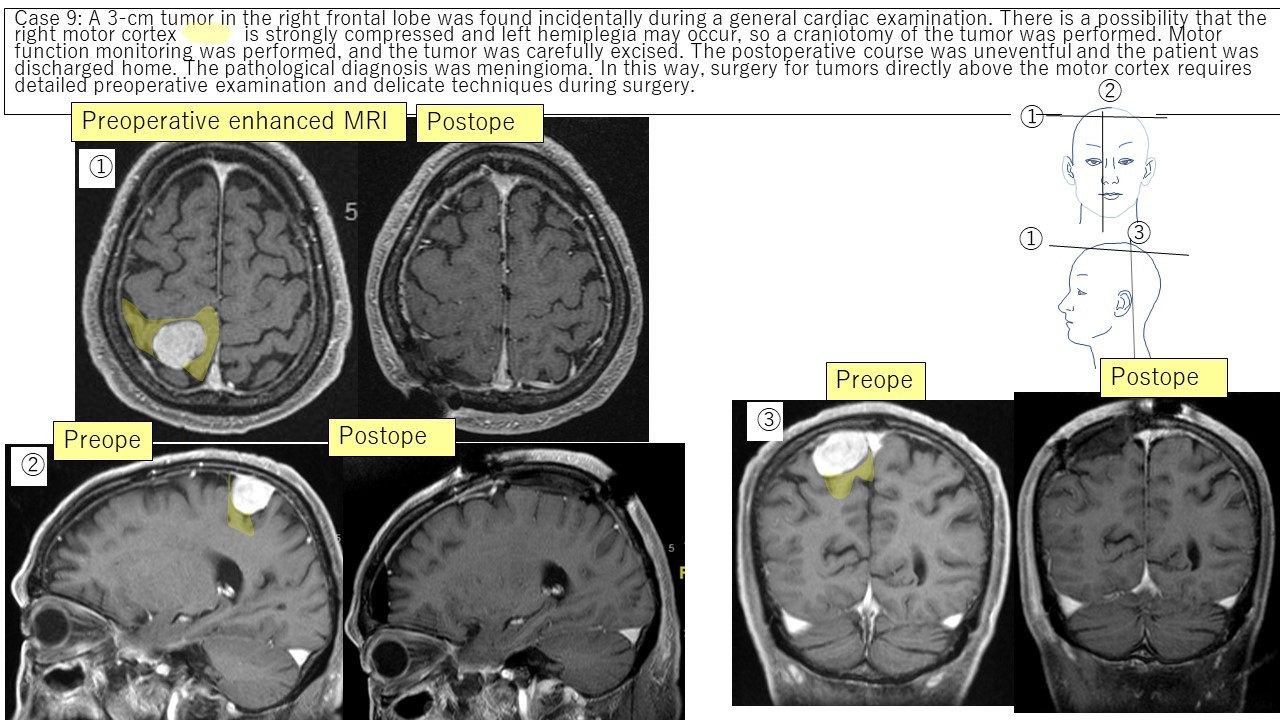
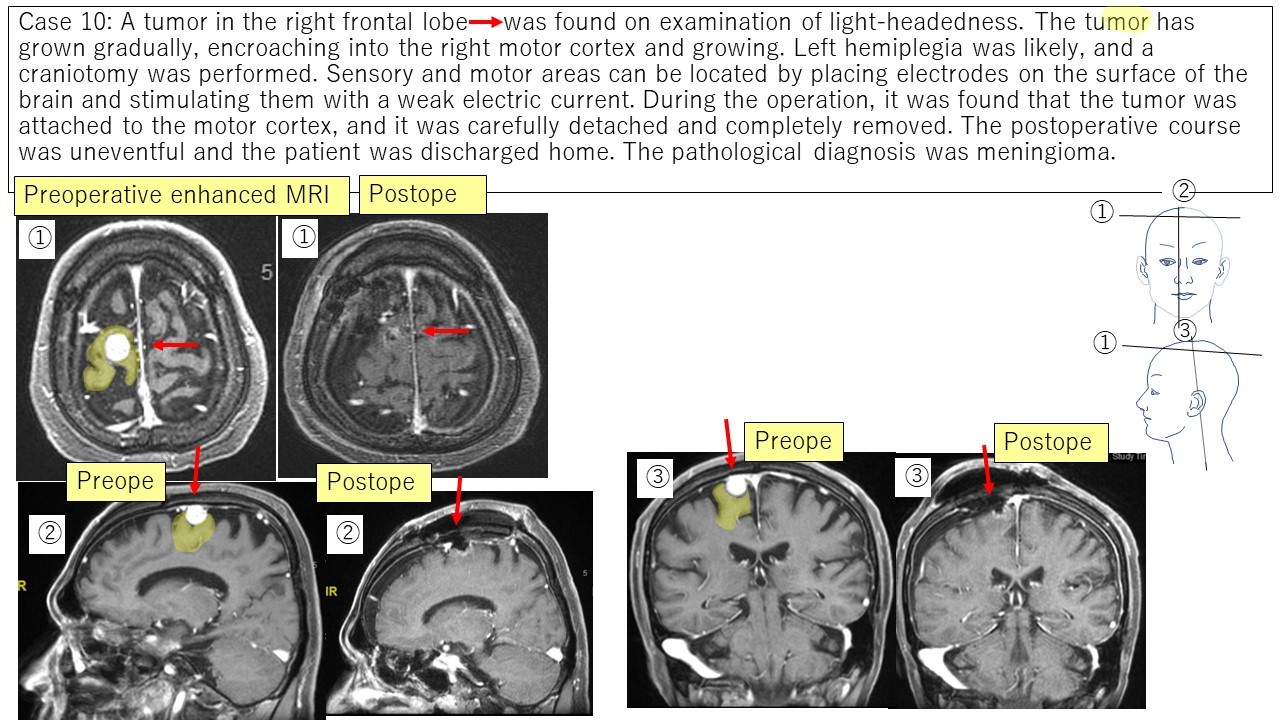
Parasagittal meningioma Case 8 Case 9 Case 10
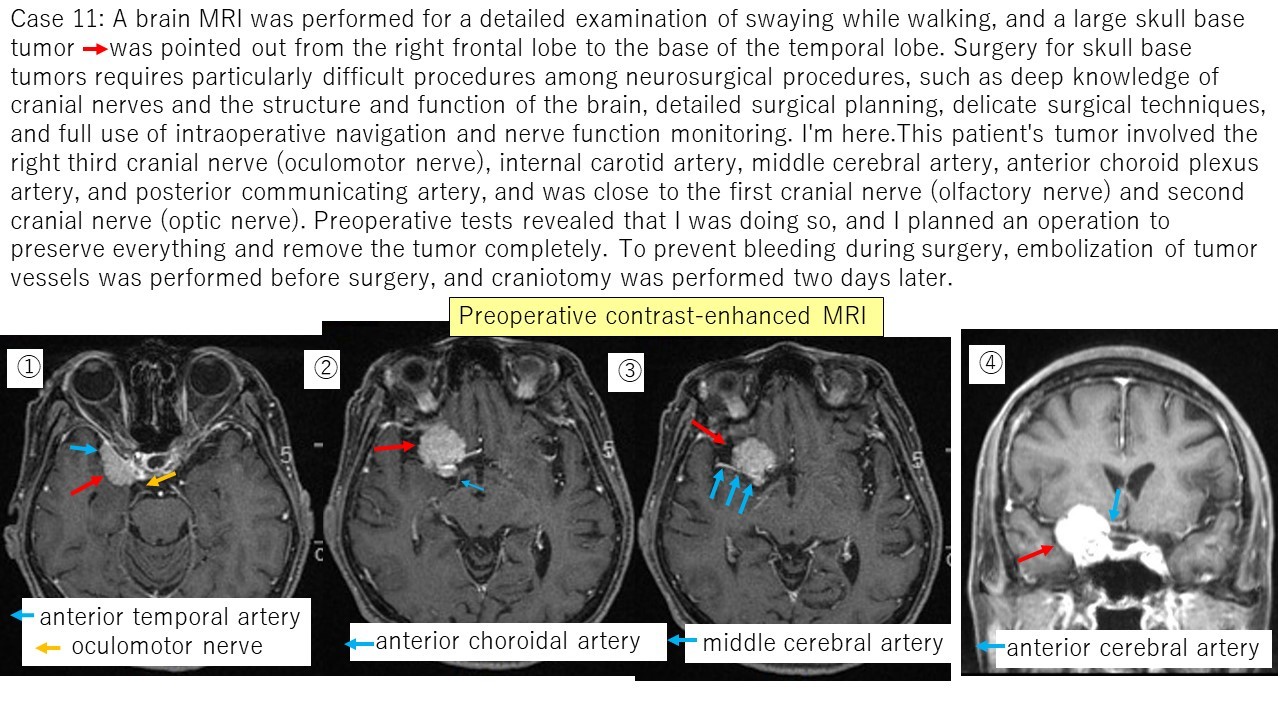
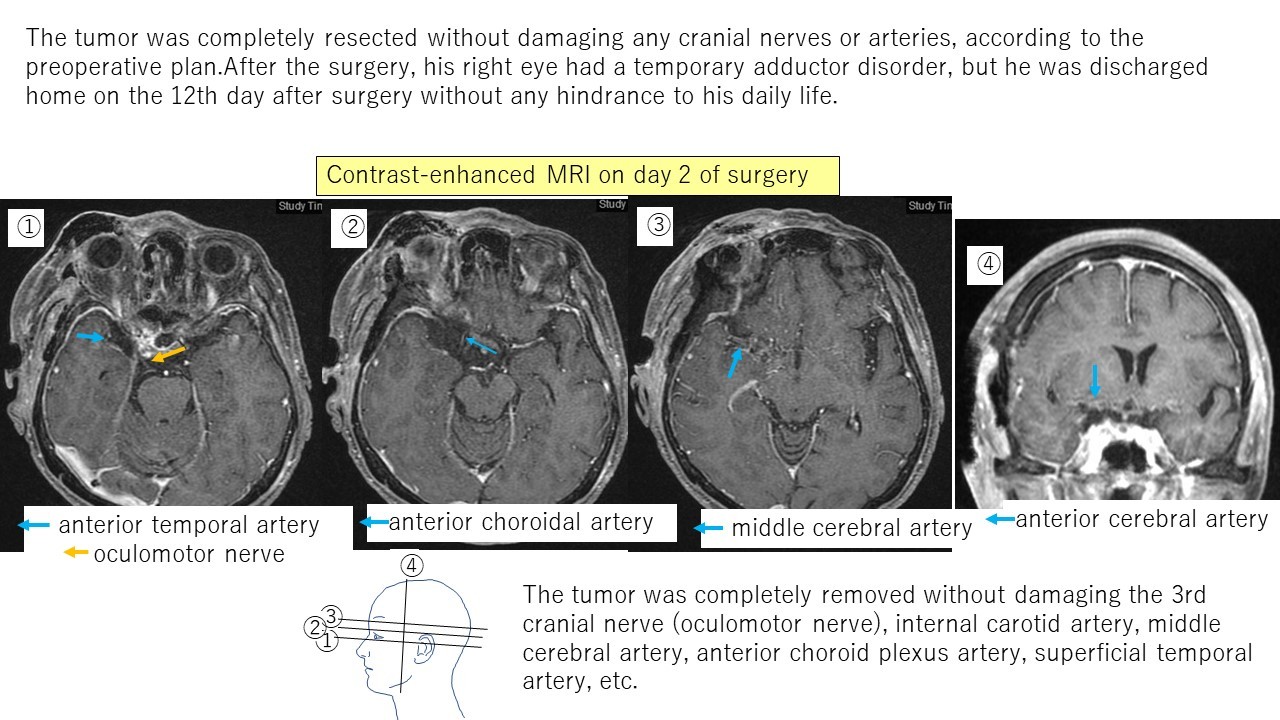
Sphenoid meningioma Case 11
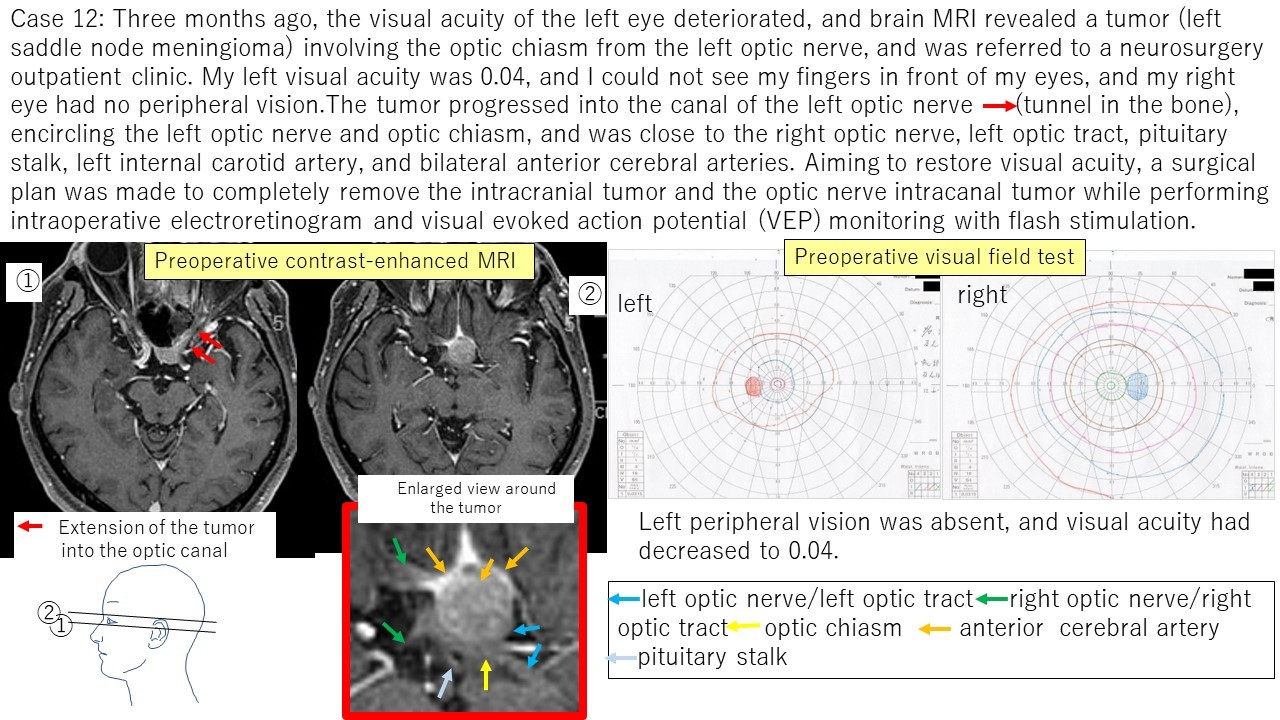
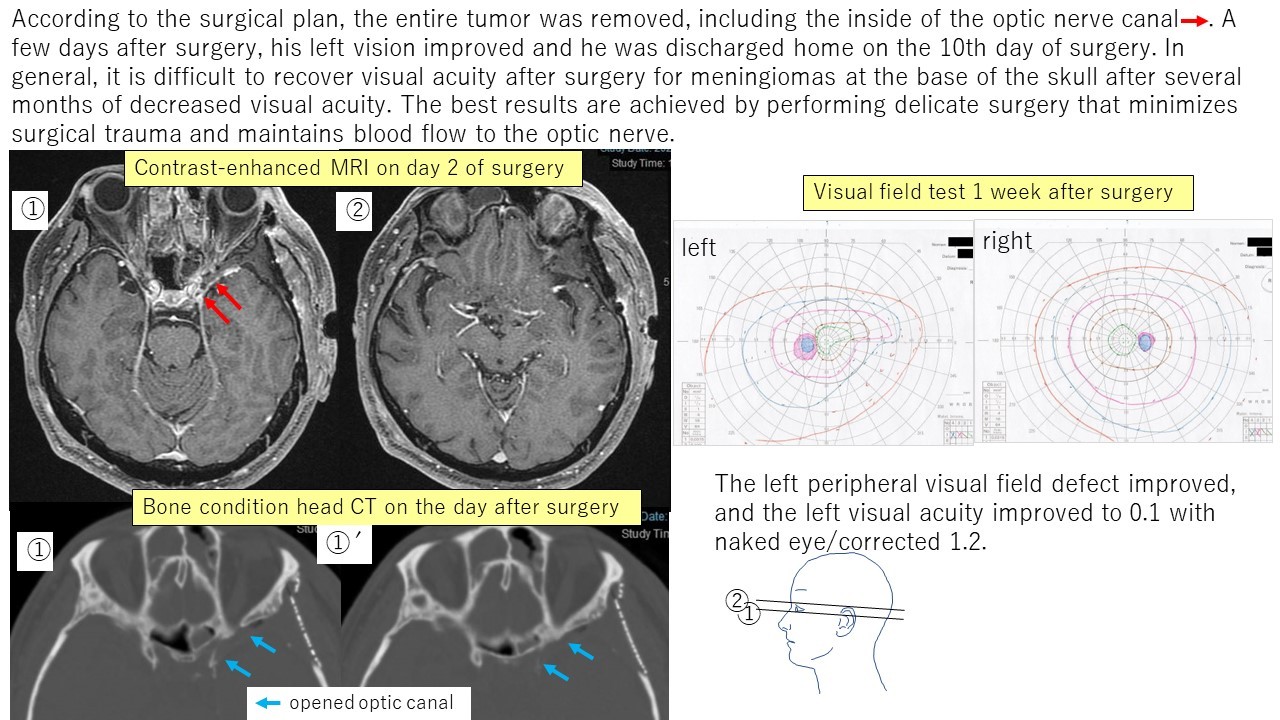
Saddle node meningioma case 12
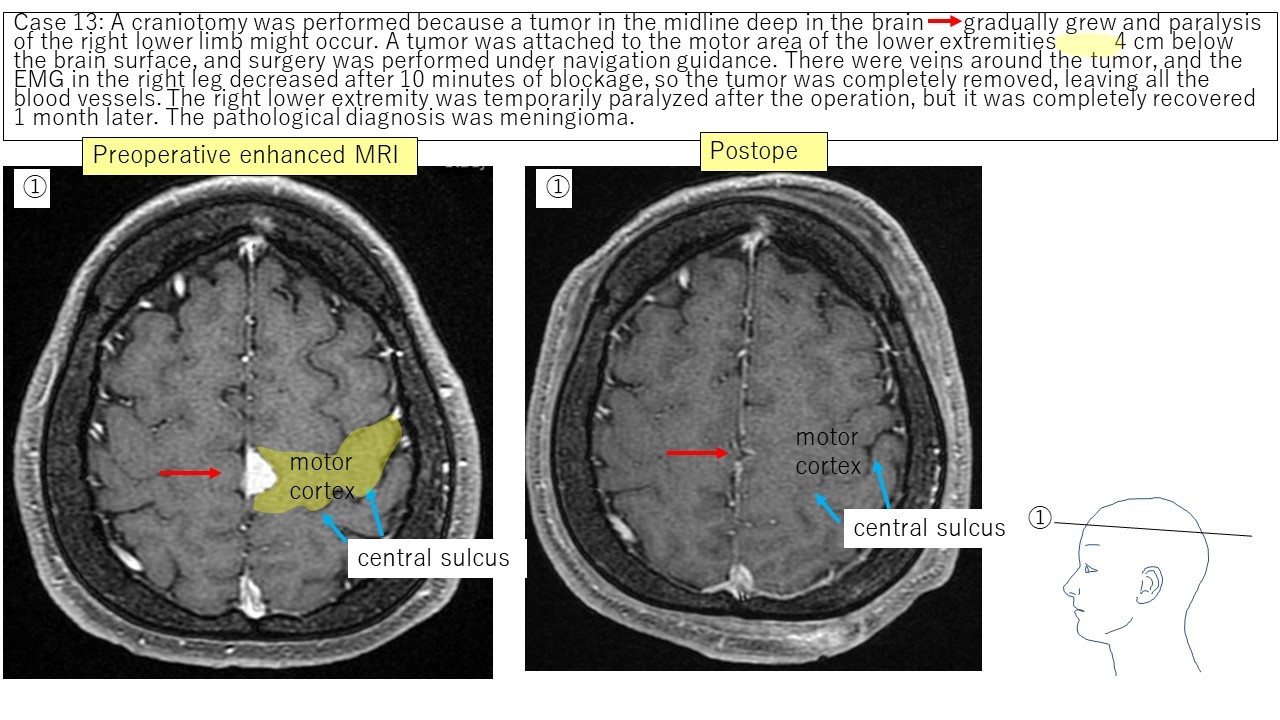
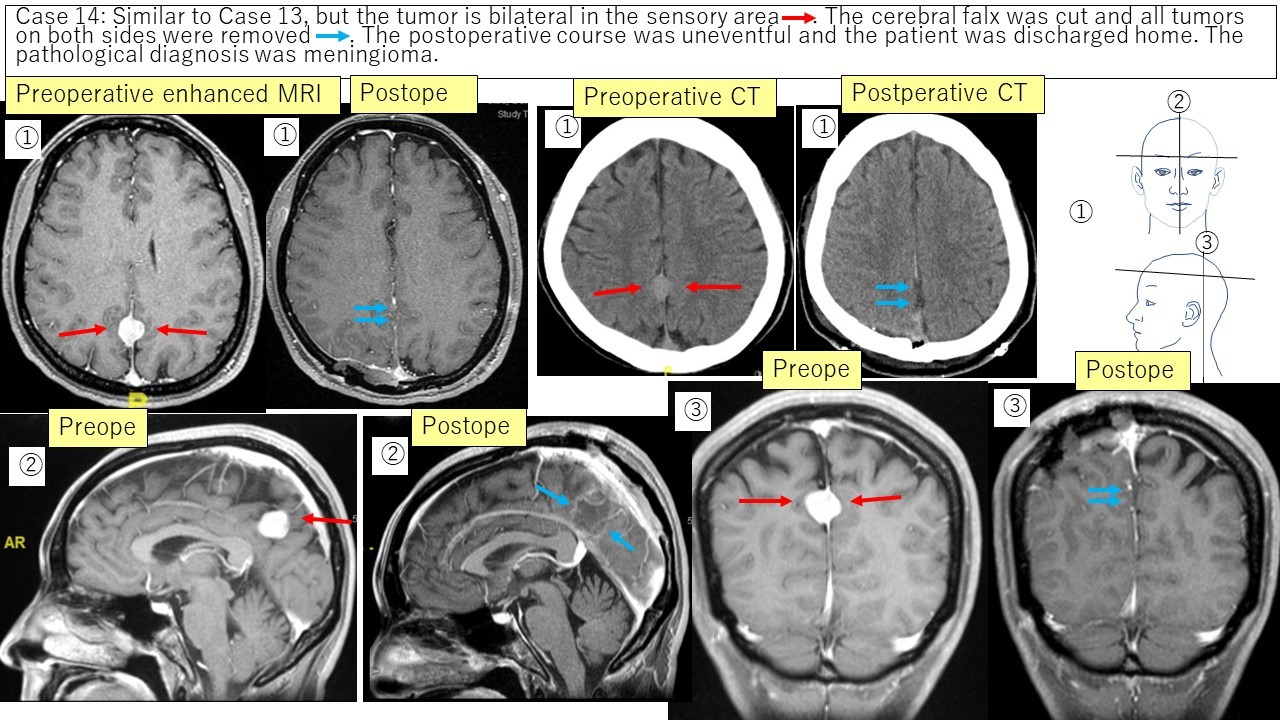
Falx meningioma Case 13 Case 14
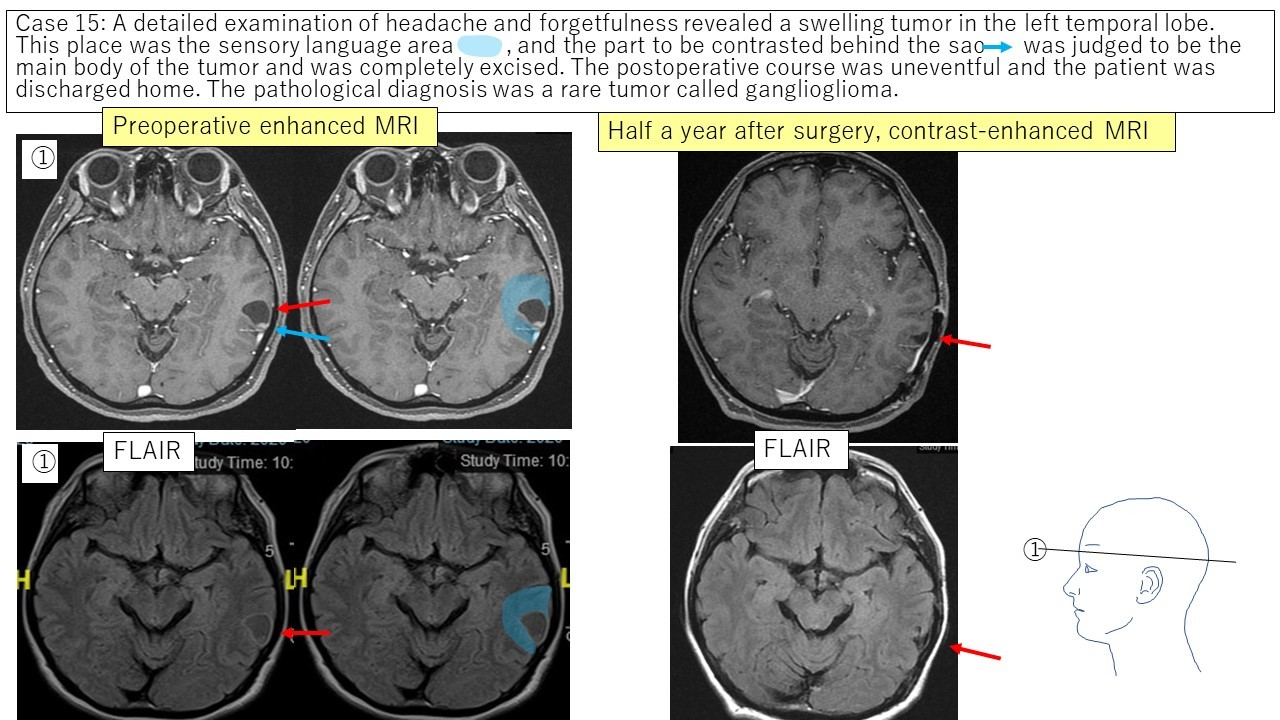
② Ganglioneuroma Case 15
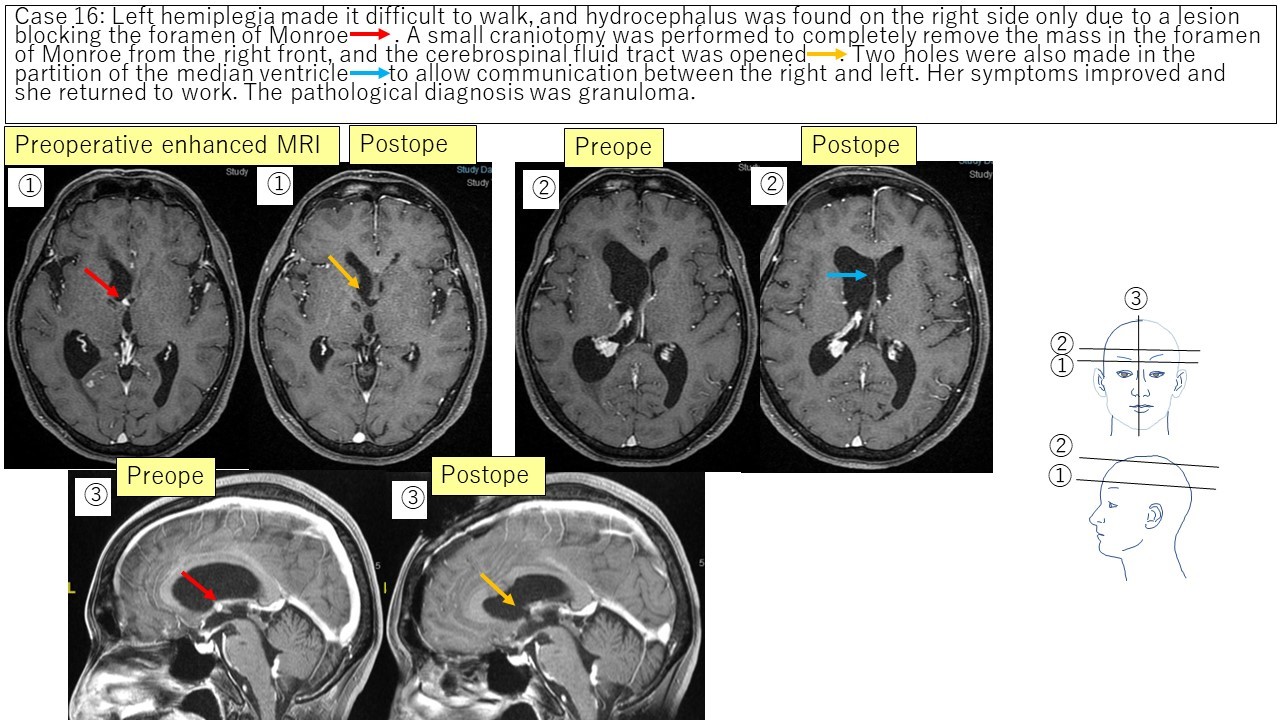
③ Intraventricular tumor (Monroe granuloma) Case 16
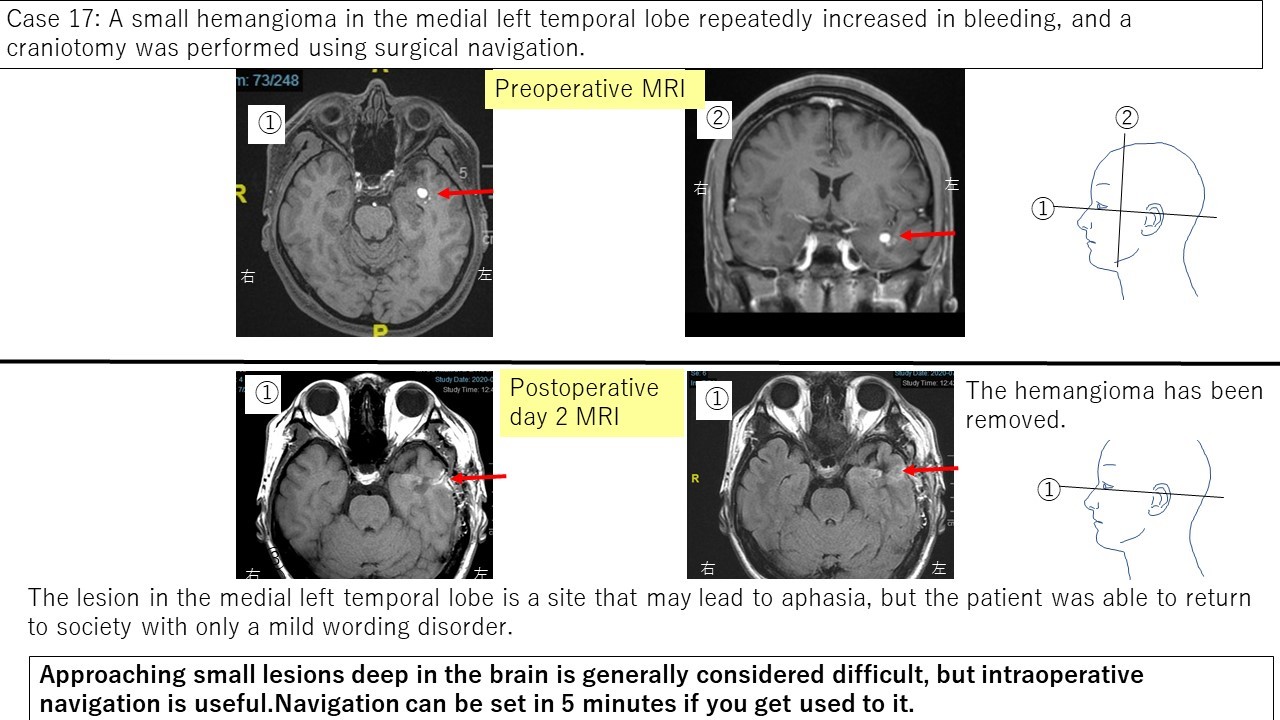
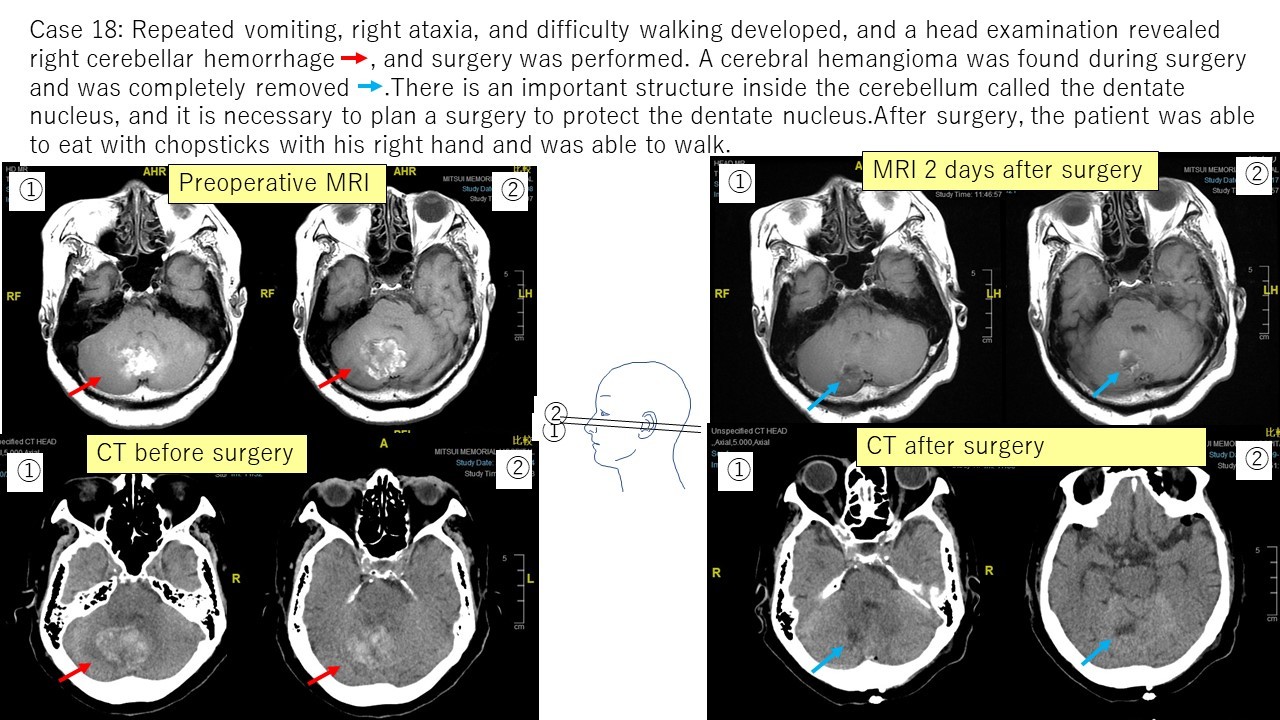
④ Hemangiomas Case 17 Case 18
In this way, I have experienced various neurosurgery operations, and I continue to study every day so that I can provide patients with appropriate diagnoses and treatments.
At the end of my self-introduction, I'm shy to show off (some of) my hobbies. As a hobby, I am most interested in getting the first grade of the Kangi character proficiensy test. I would like to get one within a few years.
⇒



 HOME (JAPANESE)
HOME (JAPANESE)







 HOME(JAPANESE)
HOME(JAPANESE) Papers/Presentation
Papers/Presentation