Cerebral infarction can occur for a variety of reasons, but it is said that the number of Japanese people suffering from cerebral infarction due to changes in dietary habits has recently increased due to stenosis or occlusion of the internal carotid artery in the neck due to atherosclerosis. Considering the current Japanese dietary habits (mainly meat dishes), it is predicted that this disease will continue to increase in the future.
If the stenosis is mild (less than 60%), treatment of atherosclerotic risk factors (hypertension, hyperlipidemia, diabetes) and lifestyle changes (e.g., avoiding tobacco, heavy drinking, and overeating), it is said to be able to stop the progression of arterial stenosis. When the stenosis becomes moderate or more (60% or more), the progression of stenosis can no longer be stopped by medical treatment, and surgery must be considered. An operation called internal carotid endarterectomy is performed, in which a vertical incision is made in the narrowed internal carotid artery, the thickened wall of the blood vessel is removed, and the artery is sewn up. If there are no particular problems, you can leave the hospital at home about two weeks after the operation.
The grounds for this are two large-scale multicenter joint studies conducted in Europe and the United States. Patients with carotid artery stenosis were divided into a group treated with oral medication alone (medical treatment group) and a group treated with carotid endarterectomy in addition to oral medication (surgical treatment group). Comparing the incidence rates, it has been proved that the surgical treatment group has better results than the medical treatment group for moderate or severe stenosis.
CEA was effective in 70% or more severe stenosis cases (50% or more in NASCET) in those with previous cerebral infarction, and 60% or more in asymptomatic cases. However, a prerequisite for these is that the surgical risk for the surgeon is low. There is no significant difference from the medical treatment group unless the surgical risk is 6% or less for symptomatic lesions and 3% or less for asymptomatic lesions.
Carotid artery stenting (CAS) may be done if CEA is a high surgical risk. In the past, carotid artery stents have not been proven to be beneficial for primary or secondary prevention of stroke like CEA, nor have they been superior to CEA. The Carotid Revascularization edarterectomy versus Stent Trial (CREST), which required the use of protective devices, demonstrated the non-inferiority of CAS in the incidence of perioperative stroke, myocardial infarction or death, and ipsilateral stroke 4 years later (Brott et al. TG, Hobson RW 2nd, Howard G, et al. NEJM 2010;365.993-1003). It has been reported that CAS has complications such as intraoperative bradycardia/hypotension, postoperative restenosis, and progression of renal failure due to contrast agents.
Figure 1: Preoperative DSA right common carotid arteriography lateral view of a 74-year-old man with cerebral infarction who developed moderate left hemiparesis and left homonymous hemianopsia. Severe stenosis of 71% was observed at the origin of the right internal carotid artery, and we considered that surgery for CEA was indicated. (NASCET method for calculating the stenosis rate = minimum diameter of blood vessel at stenotic part of internal carotid artery ÷ diameter of blood vessel at distal part of stenotic part) More than 100% vasodilation was obtained with CEA (Figure 2).
Figure 1
Figure 2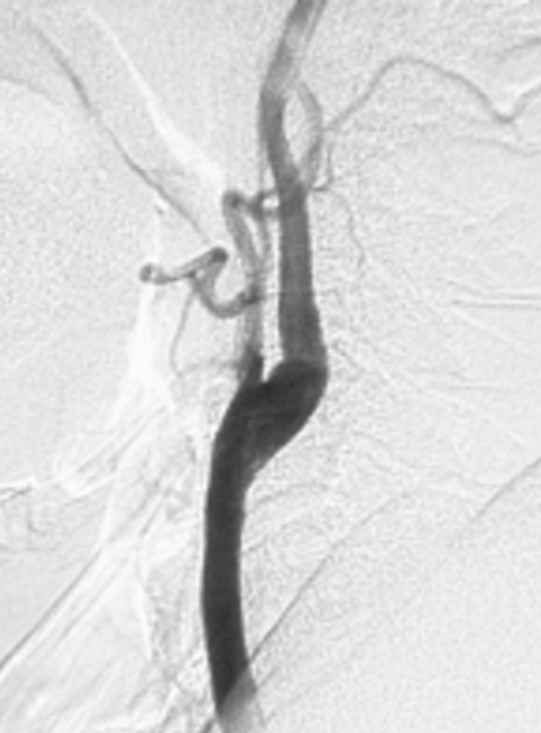
Cervical internal carotid artery stenosis can be easily diagnosed by carotid artery ultrasound during a complete medical check-up, neck MRA, etc., and can be treated before it becomes a severe cerebral infarction. If you have risk factors for arteriosclerosis and are worried about having a stroke, why not get tested?
Reference: The following two representative clinical studies have proven that CEA is more effective than medical treatment for symptomatic cervical internal carotid artery stenosis if the conditions are met.1. North American Symptomatic Carotid Endarterectomy Trial (NASCET). Started in January 1988 at 50 North American facilities. Patients with TIA or mild ischemic stroke within the past 120 days and cervical carotid artery stenosis on the affected side of 30% to 99% were randomly divided into the best medical treatment group and the best medical treatment + CEA group. This is a comparative study of the incidence of stroke between groups over a period of about two years. However, neurosurgeons performing CEA were required to have a surgical risk of 6% or less. As a result, in 1991, in the severe stenosis group of 70% or more, the incidence of stroke was 26% in the internal medicine group and 9% in the CEA group. was proven to significantly reduce the rate. Furthermore, in 1998, it was proven that the CEA group also reduced the incidence of stroke in 50-69% of patients with moderate stenosis compared to the medical treatment group. Subsequent studies proved that the CEA group had a long-term protective effect against stroke.2. European Carotid Surgery Trial (ECST): Conducted at 80 centers in 14 European countries. Patients who had a TIA or mild stroke within the past 6 months and had carotid artery stenosis on the affected side were divided into a medical group and a CEA group, and the subsequent stroke incidence was compared. . It was found that the CEA group significantly reduced the incidence of stroke compared to the internal medicine group in 70% or more cases of severe stenosis about 3 years after onset. Subsequent studies also demonstrated that the CEA group was able to reduce the incidence of stroke over the long term in patients with severe stenosis of 80% or more.For asymptomatic cervical internal carotid artery stenosis, two clinical studies have demonstrated CEA to be more beneficial than medical treatment if eligible.1. Asymptomatic Carotid Atherosclerosis Study (ACAS); performed at 39 centers in North America. Subjects were asymptomatic carotid artery stenosis with a stenosis of 60% or more. Observation period is about 5 years. The results showed that the incidence of stroke in the internal medicine group was 11.0%, while in the CEA group it was 5.1%, demonstrating the usefulness of CEA even for asymptomatic lesions. The assumption was that the surgical risk for surgeons was ≤3%.2. Asymptomatic Carotid Surgery Trial (ACST); conducted at 126 centers in 30 countries. Subjects had asymptomatic cervical carotid artery stenosis with unilateral or bilateral stenosis of 60% or more on cervical ultrasonography. significantly lower, proving CEA useful not only for men but also for women.
Snowboading head injury
coffee intake prevent silent cerebral infarction
Stroke:general information
treatment of intracerebral hemorrhage
treatment of subarachoid hemorrhage
carotid endoarterectomy
STA-MCA anastomosis
Moyamoya disease
arterio-venous malformation: AVM
MRI T2* WI
Tumor removal part 1 : FLAIR
Tumor removal part 2: navigation and monitoring
Tumor removal part 3 : approach through sulci
Tumor removal part 4 : MIB-1 labeling index



 HOME
HOME HOME JAPANESE
HOME JAPANESE Self Introduction
Self Introduction Paper/Presentation
Paper/Presentation